Optumrx, a leading pharmacy benefit management organization, requires healthcare providers to obtain prior authorization for certain medications to ensure patients receive safe and effective treatment while controlling healthcare costs. The Optumrx prior authorization form can be a daunting task for many healthcare professionals, but fear not! This comprehensive guide will break down the process into manageable steps, providing you with a clear understanding of what's required and how to navigate the system efficiently.
Understanding Prior Authorization

Prior authorization, also known as pre-authorization or pre-certification, is a process where healthcare providers must obtain approval from the patient's insurance company before prescribing specific medications or treatments. This process ensures that the prescribed treatment is medically necessary, safe, and cost-effective.
Why is Prior Authorization Necessary?
Prior authorization is necessary to:
- Ensure patient safety by verifying the prescribed treatment is appropriate for the patient's condition
- Control healthcare costs by reducing unnecessary or ineffective treatments
- Promote the use of generic or alternative medications when available
- Encourage healthcare providers to follow evidence-based treatment guidelines
Optumrx Prior Authorization Form: Step-by-Step Guide

To simplify the prior authorization process, follow these steps:
- Determine if Prior Authorization is Required: Check the Optumrx website or contact their customer service to determine if prior authorization is required for the specific medication or treatment.
- Gather Required Information: Collect the necessary patient information, including:
- Patient demographics
- Medical history
- Current medications
- Diagnosis and treatment plan
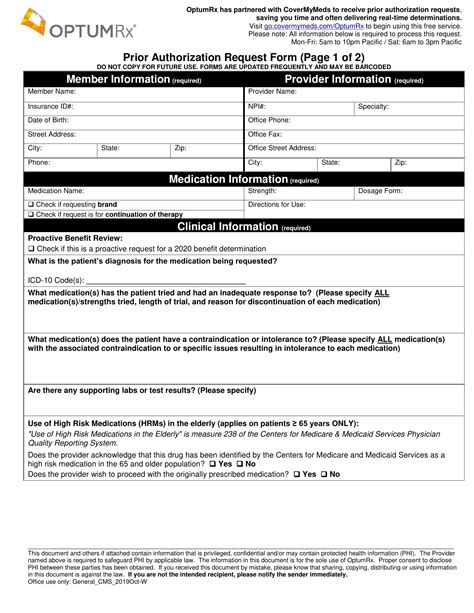
- Complete the Prior Authorization Form: Fill out the Optumrx prior authorization form, which can be downloaded from their website or obtained through their customer service. Ensure all required fields are completed accurately and thoroughly.
- Submit the Form: Fax or mail the completed form to Optumrx, following their submission guidelines.
- Await Approval or Denial: Optumrx will review the prior authorization request and respond with an approval or denial.
Common Prior Authorization Form Requirements
When completing the Optumrx prior authorization form, be sure to include the following information:
- Patient's name and date of birth
- Prescription medication or treatment details
- Diagnosis and treatment plan
- Supporting medical documentation (e.g., lab results, medical records)
Tips for a Smooth Prior Authorization Process

To ensure a seamless prior authorization process:
- Verify Patient Eligibility: Confirm the patient's insurance coverage and eligibility before submitting the prior authorization request.
- Submit Complete and Accurate Information: Ensure all required fields are completed accurately and thoroughly to avoid delays or denials.
- Follow Up: If you haven't received a response from Optumrx, follow up with their customer service to check the status of your request.
- Keep Records: Maintain a record of all prior authorization requests, including submissions, approvals, and denials.
Optumrx Prior Authorization Form FAQs

Here are some frequently asked questions about the Optumrx prior authorization form:
- Q: What is the Optumrx prior authorization form used for? A: The form is used to request approval for specific medications or treatments before they can be prescribed to patients.
- Q: How long does the prior authorization process take? A: The process typically takes 1-3 business days, but may vary depending on the complexity of the request.
- Q: Can I submit the prior authorization form electronically? A: Yes, Optumrx offers an electronic submission option through their website or through their customer service.
Conclusion: Simplifying the Optumrx Prior Authorization Process

By following this step-by-step guide and understanding the Optumrx prior authorization form requirements, you can simplify the process and ensure your patients receive the necessary medications and treatments in a timely manner. Remember to verify patient eligibility, submit complete and accurate information, and follow up on the status of your request to ensure a smooth prior authorization process.
We hope this guide has been informative and helpful. If you have any further questions or concerns, please don't hesitate to reach out. Share your experiences or tips for navigating the prior authorization process in the comments below.
What is the purpose of prior authorization?
+Prior authorization is a process where healthcare providers must obtain approval from the patient's insurance company before prescribing specific medications or treatments to ensure patient safety and control healthcare costs.
How do I know if prior authorization is required?
+Check the Optumrx website or contact their customer service to determine if prior authorization is required for the specific medication or treatment.
What information is required on the Optumrx prior authorization form?
+The form requires patient demographics, medical history, current medications, diagnosis, and treatment plan.