The process of obtaining prior authorization for Medicaid patients can be complex and time-consuming. As a healthcare provider, navigating the necessary steps to secure approval for treatments or medications is crucial to ensure that patients receive the care they need. The Nyrx Medicaid Prior Authorization Form is a critical document in this process. In this article, we will delve into the world of Medicaid prior authorization, explore the importance of the Nyrx form, and provide a comprehensive guide on how to complete it successfully.
Understanding Medicaid Prior Authorization

Prior authorization is a process used by Medicaid to determine whether a particular treatment or medication is medically necessary for a patient. This process helps ensure that patients receive only the treatments and medications that are essential for their care, while also controlling healthcare costs. The prior authorization process typically involves submitting a request to the Medicaid program, which then reviews the request to determine whether the treatment or medication is approved.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It ensures that patients receive medically necessary treatments and medications.
- It helps control healthcare costs by preventing unnecessary treatments and medications.
- It promotes the use of cost-effective treatments and medications.
The Nyrx Medicaid Prior Authorization Form

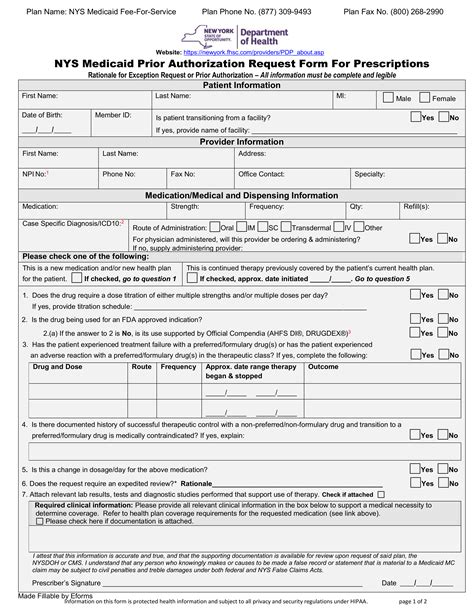
The Nyrx Medicaid Prior Authorization Form is a specific document used to request prior authorization for Medicaid patients. This form is typically completed by healthcare providers and submitted to the Medicaid program for review. The form requires detailed information about the patient, the treatment or medication being requested, and the medical necessity of the request.
Key Components of the Nyrx Form
The Nyrx Medicaid Prior Authorization Form typically includes the following key components:
- Patient information: name, date of birth, Medicaid ID number, etc.
- Treatment or medication information: name, dosage, frequency, etc.
- Medical necessity information: diagnosis, medical history, etc.
- Supporting documentation: test results, medical records, etc.
Completing the Nyrx Medicaid Prior Authorization Form

To complete the Nyrx Medicaid Prior Authorization Form successfully, follow these steps:
- Gather necessary information: Collect all relevant patient information, treatment or medication information, and medical necessity information.
- Complete the form accurately: Fill out the form completely and accurately, ensuring that all required fields are completed.
- Attach supporting documentation: Include all supporting documentation, such as test results and medical records, to support the request.
- Submit the form: Submit the completed form to the Medicaid program for review.
Tips for Successful Submission
To ensure successful submission of the Nyrx form, follow these tips:
- Verify patient eligibility: Ensure that the patient is eligible for Medicaid and that the treatment or medication is covered.
- Use clear and concise language: Use clear and concise language when completing the form to avoid confusion.
- Include all required documentation: Include all required documentation to support the request.
Common Challenges and Solutions

Completing the Nyrx Medicaid Prior Authorization Form can be challenging, but there are solutions to common problems:
- Incomplete or inaccurate information: Verify patient information and treatment or medication information to ensure accuracy.
- Missing documentation: Ensure that all required documentation is included to support the request.
- Delayed processing: Follow up with the Medicaid program to ensure timely processing of the request.
Best Practices for Streamlining the Process
To streamline the prior authorization process, follow these best practices:
- Use electronic submission: Use electronic submission to reduce paperwork and increase efficiency.
- Use a prior authorization software: Use a prior authorization software to automate the process and reduce errors.
- Designate a prior authorization coordinator: Designate a prior authorization coordinator to manage the process and ensure timely submission.
Conclusion

In conclusion, the Nyrx Medicaid Prior Authorization Form is a critical document in the prior authorization process. By understanding the importance of prior authorization, completing the form accurately, and following best practices, healthcare providers can ensure that patients receive the care they need while also controlling healthcare costs.
We encourage you to share your experiences and tips for completing the Nyrx Medicaid Prior Authorization Form in the comments below.
What is the purpose of the Nyrx Medicaid Prior Authorization Form?
+The Nyrx Medicaid Prior Authorization Form is used to request prior authorization for Medicaid patients. It provides detailed information about the patient, the treatment or medication being requested, and the medical necessity of the request.
What information is required on the Nyrx form?
+The Nyrx form requires patient information, treatment or medication information, medical necessity information, and supporting documentation.
How can I ensure successful submission of the Nyrx form?
+To ensure successful submission, verify patient eligibility, use clear and concise language, and include all required documentation.