In the healthcare industry, prior authorization is a crucial process that ensures patients receive necessary medical treatment while also helping to manage healthcare costs. One essential document required for this process is the Nia Prior Authorization Form. In this article, we will explore the significance of this form, its components, and provide a step-by-step guide on how to complete it efficiently.
Understanding the Nia Prior Authorization Form

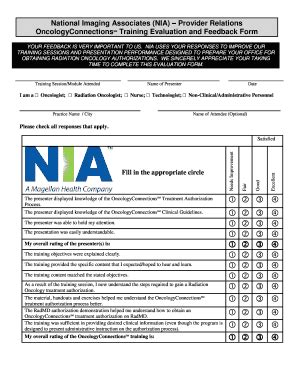
The Nia Prior Authorization Form is a critical document that healthcare providers must complete to request approval for specific medical treatments, services, or medications. This form helps ensure that patients receive necessary care while also enabling healthcare payers to manage costs and ensure that treatments are medically necessary.
Components of the Nia Prior Authorization Form
Before we dive into the completion process, it's essential to understand the key components of the Nia Prior Authorization Form:
- Patient information: name, date of birth, and contact details
- Healthcare provider information: name, contact details, and credentials
- Medical treatment or service information: description, diagnosis, and treatment plan
- Supporting documentation: medical records, test results, and other relevant documents
5 Ways to Complete the Nia Prior Authorization Form

Completing the Nia Prior Authorization Form requires attention to detail, accuracy, and efficiency. Here are five ways to complete the form efficiently:
1. Gather Required Information and Documentation
Before starting the form, ensure you have all the necessary patient information, medical records, and supporting documentation. This will help you complete the form accurately and efficiently.
2. Use Clear and Concise Language
When describing the medical treatment or service, use clear and concise language to ensure that the healthcare payer understands the request. Avoid using jargon or technical terms that may be unfamiliar to non-medical professionals.
3. Provide Detailed Supporting Documentation
Supporting documentation is crucial in the prior authorization process. Ensure that you provide detailed medical records, test results, and other relevant documents that support the requested treatment or service.
4. Complete the Form Electronically or Manually
The Nia Prior Authorization Form can be completed electronically or manually. If completing the form manually, ensure that you use black ink and write legibly. If completing the form electronically, ensure that you use a secure and compliant platform.
5. Review and Submit the Form Accurately
Before submitting the form, review it carefully to ensure that all information is accurate and complete. Verify that all required fields are filled, and supporting documentation is attached. Submit the form to the healthcare payer in a timely manner to avoid delays in the approval process.
Tips for Efficient Form Completion
- Use a template or example form to guide you through the completion process
- Ensure that all patient information is accurate and up-to-date
- Use a secure and compliant platform for electronic form completion
- Verify that all supporting documentation is complete and accurate
- Submit the form in a timely manner to avoid delays in the approval process
Benefits of Efficient Prior Authorization

Efficient prior authorization can bring numerous benefits to healthcare providers, payers, and patients. Some of these benefits include:
- Improved patient outcomes: efficient prior authorization ensures that patients receive necessary medical treatment in a timely manner
- Reduced administrative burden: streamlining the prior authorization process reduces administrative tasks and costs
- Enhanced patient satisfaction: efficient prior authorization reduces delays and frustration for patients
- Cost savings: efficient prior authorization helps manage healthcare costs by ensuring that treatments are medically necessary
Common Challenges in Prior Authorization

Despite the benefits of prior authorization, there are common challenges that healthcare providers and payers face. Some of these challenges include:
- Complexity of the prior authorization process
- Lack of standardization in prior authorization forms and processes
- Insufficient communication between healthcare providers and payers
- Delays in the approval process
Overcoming Prior Authorization Challenges
- Implementing efficient and standardized prior authorization processes
- Enhancing communication between healthcare providers and payers
- Providing education and training for healthcare providers on prior authorization best practices
- Utilizing technology to streamline the prior authorization process
Conclusion and Next Steps

Completing the Nia Prior Authorization Form efficiently requires attention to detail, accuracy, and efficiency. By following the five ways outlined in this article, healthcare providers can streamline the prior authorization process, reduce administrative burden, and improve patient outcomes.
If you're a healthcare provider looking to improve your prior authorization process, consider the following next steps:
- Review and update your prior authorization processes to ensure efficiency and standardization
- Educate and train your staff on prior authorization best practices
- Utilize technology to streamline the prior authorization process
- Communicate with healthcare payers to ensure timely and accurate approval
By taking these steps, you can improve the prior authorization process, reduce administrative burden, and enhance patient satisfaction.
What is the purpose of the Nia Prior Authorization Form?
+The Nia Prior Authorization Form is used to request approval for specific medical treatments, services, or medications. It helps ensure that patients receive necessary care while also enabling healthcare payers to manage costs and ensure that treatments are medically necessary.
What information is required to complete the Nia Prior Authorization Form?
+The form requires patient information, healthcare provider information, medical treatment or service information, and supporting documentation.
How can I overcome common challenges in prior authorization?
+Implementing efficient and standardized prior authorization processes, enhancing communication between healthcare providers and payers, providing education and training for healthcare providers on prior authorization best practices, and utilizing technology to streamline the prior authorization process can help overcome common challenges.