Prior authorization is a crucial process in the healthcare industry that ensures patients receive the necessary treatment while also controlling healthcare costs. One of the prominent healthcare companies that use prior authorization forms is Molina Healthcare. If you are a healthcare provider or a patient, you may need to fill out a Molina prior authorization form to obtain approval for certain treatments or services.
In this comprehensive guide, we will walk you through the Molina prior authorization form, including its importance, how to fill it out, and where to download the form.
What is a Prior Authorization Form?

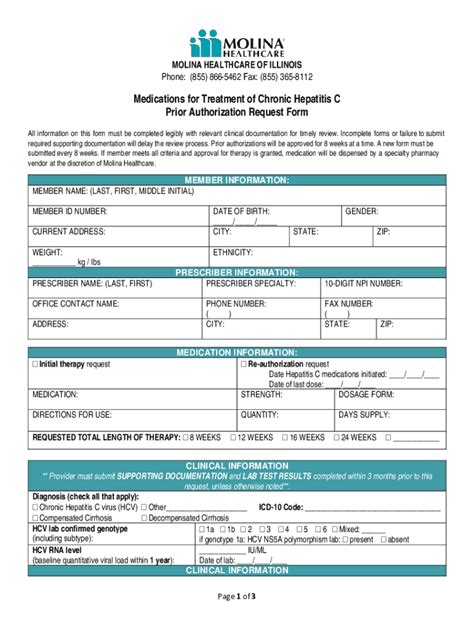
A prior authorization form, also known as a pre-authorization or pre-certification form, is a document that healthcare providers must fill out and submit to a patient's insurance company before rendering certain medical services or prescribing specific medications. The form provides the insurance company with detailed information about the proposed treatment, including the patient's medical history, diagnosis, and the rationale behind the treatment.
The primary purpose of a prior authorization form is to ensure that the proposed treatment is medically necessary and aligns with the insurance company's coverage policies. This process helps to prevent unnecessary medical expenses and ensures that patients receive the most effective and cost-efficient care.
Why is the Molina Prior Authorization Form Important?

The Molina prior authorization form is essential for both healthcare providers and patients. Here are some reasons why:
- Ensures medically necessary treatment: The form helps to ensure that patients receive only medically necessary treatments, which reduces the risk of unnecessary medical expenses and improves health outcomes.
- Streamlines the approval process: The form provides a standardized way for healthcare providers to submit prior authorization requests, which streamlines the approval process and reduces administrative burdens.
- Improves patient satisfaction: By ensuring that patients receive timely and effective treatment, the prior authorization form helps to improve patient satisfaction and health outcomes.
- Reduces healthcare costs: The form helps to reduce healthcare costs by preventing unnecessary medical expenses and promoting cost-efficient care.
How to Fill Out the Molina Prior Authorization Form

Filling out the Molina prior authorization form requires attention to detail and accurate information. Here are the steps to follow:
- Download the form: You can download the Molina prior authorization form from the Molina Healthcare website or obtain it from your healthcare provider.
- Gather required information: Collect the patient's medical records, including their medical history, diagnosis, and treatment plan.
- Fill out the form: Complete the form with accurate and detailed information, including the patient's demographics, medical history, and treatment plan.
- Attach supporting documentation: Attach supporting documentation, such as medical records and test results, to the form.
- Submit the form: Submit the completed form to Molina Healthcare for review and approval.
Where to Download the Molina Prior Authorization Form

You can download the Molina prior authorization form from the Molina Healthcare website or obtain it from your healthcare provider. Here are the steps to follow:
- Visit the Molina Healthcare website: Go to the Molina Healthcare website and click on the "Providers" tab.
- Click on "Prior Authorization": Click on the "Prior Authorization" link and select the type of prior authorization form you need.
- Download the form: Download the form and save it to your computer.
- Print the form: Print the form and fill it out with accurate and detailed information.
Alternatively, you can obtain the Molina prior authorization form from your healthcare provider. They may have a copy of the form or be able to provide you with a link to download it.
Common Questions and Answers
Here are some common questions and answers about the Molina prior authorization form:
What is the purpose of the Molina prior authorization form?
The purpose of the Molina prior authorization form is to ensure that patients receive medically necessary treatment and to control healthcare costs.
How do I fill out the Molina prior authorization form?
To fill out the Molina prior authorization form, gather the required information, fill out the form with accurate and detailed information, attach supporting documentation, and submit the form to Molina Healthcare for review and approval.
Where can I download the Molina prior authorization form?
You can download the Molina prior authorization form from the Molina Healthcare website or obtain it from your healthcare provider.
What is the Molina prior authorization form used for?
+The Molina prior authorization form is used to request approval for certain medical services or treatments.
How long does it take to get approved for prior authorization?
+The approval process typically takes 24-48 hours, but it may vary depending on the complexity of the request.
Can I fax the prior authorization form to Molina Healthcare?
+Yes, you can fax the prior authorization form to Molina Healthcare, but it is recommended to submit it electronically or by mail to ensure timely processing.
By following the guidelines outlined in this article, you can ensure that you fill out the Molina prior authorization form correctly and efficiently. Remember to gather all the required information, fill out the form with accurate and detailed information, and attach supporting documentation to ensure a smooth approval process. If you have any questions or concerns, don't hesitate to reach out to Molina Healthcare or your healthcare provider for assistance.