As a healthcare provider in Texas, you're likely familiar with the prior authorization process for Molina Healthcare. Prior authorization, also known as pre-authorization or pre-certification, is a process that ensures patients receive medically necessary care while controlling healthcare costs. In this article, we'll delve into the world of Molina prior authorization in Texas, providing you with an easy-to-follow guide.
Understanding Molina Prior Authorization in Texas

Molina Healthcare is a health insurance company that provides coverage to millions of Americans, including those in Texas. To ensure that patients receive necessary care while managing costs, Molina has implemented a prior authorization process. This process requires healthcare providers to obtain approval from Molina before performing certain medical procedures or prescribing specific medications.
Why is Prior Authorization Necessary?
Prior authorization is essential for several reasons:
- Cost control: By reviewing medical procedures and prescriptions before they're administered, Molina can ensure that patients receive necessary care while avoiding unnecessary costs.
- Quality of care: Prior authorization helps ensure that patients receive high-quality care that aligns with established medical standards.
- Patient safety: By reviewing medical procedures and prescriptions, Molina can help prevent adverse reactions, allergic reactions, and other safety issues.
The Molina Prior Authorization Process in Texas

The Molina prior authorization process in Texas involves several steps:
- Check the Molina website: Before submitting a prior authorization request, check the Molina website to see if the procedure or medication requires prior authorization.
- Submit the request: Submit the prior authorization request via phone, fax, or online portal. Make sure to include all required documentation, such as patient information, medical records, and treatment plans.
- Review and approval: Molina will review the request and approve or deny it based on medical necessity and established guidelines.
- Notification: Molina will notify the healthcare provider and patient of the approval or denial decision.
Required Documents for Molina Prior Authorization in Texas
To ensure a smooth prior authorization process, make sure to include the following documents:
- Patient information: Include patient demographics, medical history, and current treatment plans.
- Medical records: Provide relevant medical records, such as test results, diagnoses, and treatment outcomes.
- Prescription information: Include prescription details, such as medication names, dosages, and frequencies.
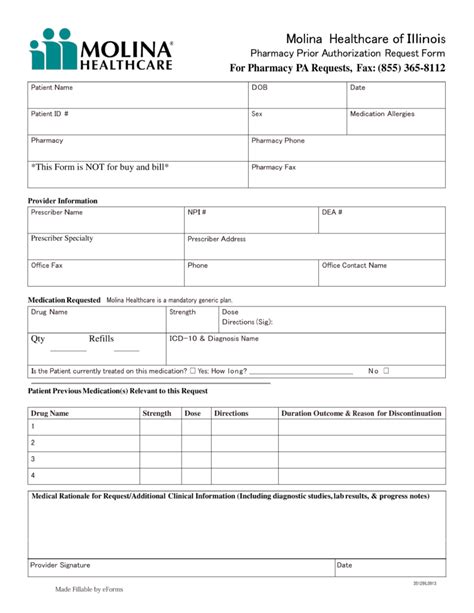
Molina Prior Authorization Form Texas

The Molina prior authorization form for Texas can be found on the Molina website or by contacting Molina customer service. The form typically requires the following information:
- Patient demographics: Include patient name, date of birth, and contact information.
- Medical procedure or medication: Describe the medical procedure or medication being requested.
- Medical justification: Provide a clear medical justification for the requested procedure or medication.
Common Challenges and Solutions
Despite the importance of prior authorization, healthcare providers may encounter challenges during the process. Here are some common challenges and solutions:
- Delays in approval: To avoid delays, ensure that all required documentation is included with the prior authorization request.
- Denial of requests: If a request is denied, review the denial reason and resubmit the request with additional information or clarification.
Best Practices for Molina Prior Authorization in Texas

To ensure a smooth prior authorization process, follow these best practices:
- Verify patient eligibility: Verify patient eligibility before submitting a prior authorization request.
- Use the correct form: Use the correct prior authorization form for Texas and ensure it's completed accurately.
- Include all required documentation: Include all required documentation, such as patient information, medical records, and prescription information.
Conclusion
Molina prior authorization in Texas is an essential process that ensures patients receive necessary care while managing costs. By understanding the prior authorization process, required documents, and best practices, healthcare providers can navigate the process with ease. Remember to verify patient eligibility, use the correct form, and include all required documentation to avoid delays and denials.
What is prior authorization, and why is it necessary?
+Prior authorization is a process that ensures patients receive medically necessary care while controlling healthcare costs. It's necessary to ensure quality of care, patient safety, and cost control.
How do I submit a prior authorization request to Molina?
+You can submit a prior authorization request via phone, fax, or online portal. Make sure to include all required documentation, such as patient information, medical records, and treatment plans.
What are some common challenges and solutions for Molina prior authorization in Texas?
+Common challenges include delays in approval and denial of requests. Solutions include ensuring all required documentation is included with the prior authorization request and reviewing denial reasons before resubmitting the request.