As a healthcare provider in Ohio, navigating the complexities of prior authorization can be a daunting task. One crucial step in this process is completing the Molina prior authorization form, which is essential for ensuring that your patients receive the necessary medical treatment. In this article, we will break down the Molina prior authorization form Ohio into 5 easy steps, providing you with a comprehensive guide on how to complete it efficiently.

Understanding the Importance of Prior Authorization
Prior authorization is a process that allows healthcare providers to obtain approval from insurance companies before providing specific medical treatments or services. This process helps to ensure that patients receive necessary and cost-effective care. Molina Healthcare, a leading health insurance provider in Ohio, requires prior authorization for certain medical services to ensure that patients receive the best possible care.
Step 1: Gather Required Information
Before starting the prior authorization process, it's essential to gather all the necessary information. This includes:
- Patient demographics, including name, date of birth, and insurance ID number
- Detailed description of the medical service or treatment being requested
- Diagnosis code(s) and relevant medical history
- Prescription medication list (if applicable)
- Contact information for the healthcare provider and patient
Having this information readily available will help streamline the prior authorization process.
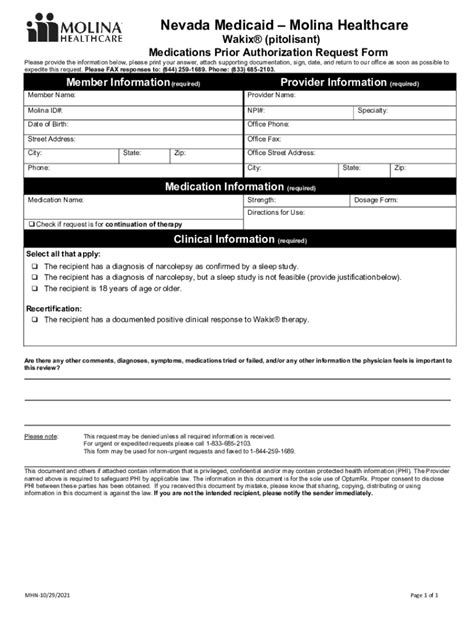
**Step 2: Choose the Correct Form**
Molina Healthcare provides various prior authorization forms for different medical services. It's crucial to select the correct form for the specific service being requested. You can find the forms on the Molina Healthcare website or by contacting their customer service department.

Step 3: Complete the Form Accurately
Once you have selected the correct form, complete it accurately and thoroughly. Make sure to:
- Fill in all required fields, including patient demographics and medical information
- Provide a clear and concise description of the medical service or treatment being requested
- Attach supporting documentation, such as medical records or test results (if applicable)
- Sign and date the form
Incomplete or inaccurate forms may result in delays or denials of prior authorization.
**Tips for Completing the Form**
- Use black ink to fill out the form
- Make sure to include all required attachments
- Keep a copy of the completed form for your records
**Step 4: Submit the Form**
After completing the form, submit it to Molina Healthcare via fax, email, or mail. Make sure to follow the submission guidelines outlined on the form or on the Molina Healthcare website.

Step 5: Follow Up on the Status
After submitting the prior authorization form, follow up with Molina Healthcare to confirm receipt and check on the status of the request. You can do this by contacting their customer service department or checking the status online through the Molina Healthcare provider portal.
**What to Expect After Submission**
- Molina Healthcare will review the prior authorization request and may contact you for additional information
- You will receive a determination letter indicating approval or denial of the request
- If approved, the patient will receive the necessary medical treatment or service
By following these 5 easy steps, you can efficiently complete the Molina prior authorization form Ohio and ensure that your patients receive the necessary medical treatment. Remember to stay organized, provide accurate information, and follow up on the status to ensure a smooth prior authorization process.
We hope this article has provided you with a comprehensive guide on how to complete the Molina prior authorization form Ohio. If you have any further questions or concerns, please don't hesitate to reach out.
What is prior authorization?
+Prior authorization is a process that allows healthcare providers to obtain approval from insurance companies before providing specific medical treatments or services.
How long does the prior authorization process take?
+The prior authorization process typically takes 3-5 business days, but may vary depending on the complexity of the request and the availability of information.
Can I submit the prior authorization form electronically?
+Yes, Molina Healthcare allows electronic submission of prior authorization forms through their provider portal.