The Molina prior authorization form is a crucial document that healthcare providers must complete to obtain approval for certain medical treatments, services, or medications for patients enrolled in Molina Healthcare plans. Completing this form accurately and efficiently can help ensure timely approval and minimize delays in patient care. In this article, we will break down the Molina prior authorization form process into 5 easy steps, providing you with a comprehensive guide to navigate this often-daunting task.

Understanding the Molina Prior Authorization Form
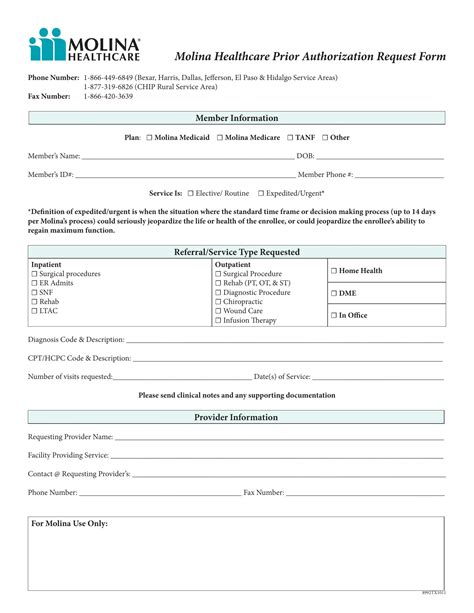
Before diving into the step-by-step guide, it's essential to understand the purpose and importance of the Molina prior authorization form. This form serves as a request for Molina Healthcare to review and approve specific medical services or treatments that are not automatically covered under the patient's healthcare plan. The form requires healthcare providers to provide detailed information about the patient's condition, treatment plan, and rationale for the requested services.
What Information is Required on the Molina Prior Authorization Form?
The Molina prior authorization form typically requires the following information:
- Patient demographics and identifying information
- Medical history and current condition
- Treatment plan and requested services
- Rationale for the requested services
- Supporting documentation, such as medical records and test results
Step 1: Gather Required Information and Documentation

The first step in completing the Molina prior authorization form is to gather all required information and documentation. This includes:
- Patient demographics and identifying information
- Medical history and current condition
- Treatment plan and requested services
- Supporting documentation, such as medical records and test results
It's essential to ensure that all information is accurate and up-to-date to avoid delays or denials.
Tips for Gathering Information:
- Verify patient information and demographics
- Review medical history and current condition
- Ensure treatment plan and requested services are clearly documented
- Collect all supporting documentation, including medical records and test results
Step 2: Complete the Molina Prior Authorization Form

Once you have gathered all required information and documentation, it's time to complete the Molina prior authorization form. This involves filling out the form accurately and thoroughly, ensuring that all required fields are completed.
Tips for Completing the Form:
- Read the form carefully and follow instructions
- Complete all required fields
- Ensure accurate and thorough documentation
- Review the form for errors or omissions
Step 3: Submit the Molina Prior Authorization Form

After completing the Molina prior authorization form, it's time to submit it to Molina Healthcare for review. This can be done via fax, mail, or online portal, depending on the specific requirements.
Tips for Submitting the Form:
- Verify submission requirements and deadlines
- Ensure accurate and complete submission
- Retain a copy of the submitted form for records
Step 4: Follow Up on the Status of the Molina Prior Authorization Form

After submitting the Molina prior authorization form, it's essential to follow up on the status of the request. This can be done by contacting Molina Healthcare's customer service or checking the online portal.
Tips for Following Up:
- Verify the status of the request
- Address any issues or concerns
- Ensure timely resolution and approval
Step 5: Review and Implement the Molina Prior Authorization Form Decision

The final step is to review and implement the decision made by Molina Healthcare regarding the prior authorization form. This involves reviewing the approval or denial letter and taking necessary actions.
Tips for Reviewing and Implementing the Decision:
- Review the approval or denial letter carefully
- Understand the rationale for the decision
- Implement the approved treatment plan or appeal the denial
By following these 5 easy steps, healthcare providers can efficiently and accurately complete the Molina prior authorization form, ensuring timely approval and minimizing delays in patient care.
What is the purpose of the Molina prior authorization form?
+The Molina prior authorization form is a request for Molina Healthcare to review and approve specific medical services or treatments that are not automatically covered under the patient's healthcare plan.
What information is required on the Molina prior authorization form?
+The form requires patient demographics and identifying information, medical history and current condition, treatment plan and requested services, rationale for the requested services, and supporting documentation.
How do I submit the Molina prior authorization form?
+The form can be submitted via fax, mail, or online portal, depending on the specific requirements.
We hope this article has provided you with a comprehensive guide to completing the Molina prior authorization form. By following these 5 easy steps, you can ensure timely approval and minimize delays in patient care. If you have any questions or concerns, please don't hesitate to reach out to Molina Healthcare's customer service.