The world of healthcare can be complex and overwhelming, especially when it comes to navigating the process of prior authorization for medications. For patients, healthcare providers, and insurance companies alike, understanding the intricacies of prior authorization can be a daunting task. However, with the Molina prior authorization form, the process of obtaining approval for necessary medications has become more streamlined and efficient. In this article, we will delve into the world of prior authorization, exploring the benefits, working mechanisms, and steps involved in utilizing the Molina prior authorization form.
Understanding Prior Authorization

Prior authorization is a process used by insurance companies to determine whether a specific medication or treatment is medically necessary and covered under a patient's insurance plan. This process is designed to ensure that patients receive safe and effective treatments while also controlling healthcare costs. Prior authorization typically involves the healthcare provider submitting a request to the insurance company, which then reviews the request and makes a determination.
The Benefits of Prior Authorization
Prior authorization offers several benefits for patients, healthcare providers, and insurance companies. Some of these benefits include:
- Ensures that patients receive safe and effective treatments
- Helps control healthcare costs by reducing unnecessary treatments
- Streamlines the process of obtaining approval for medications
- Enhances communication between healthcare providers and insurance companies
The Molina Prior Authorization Form

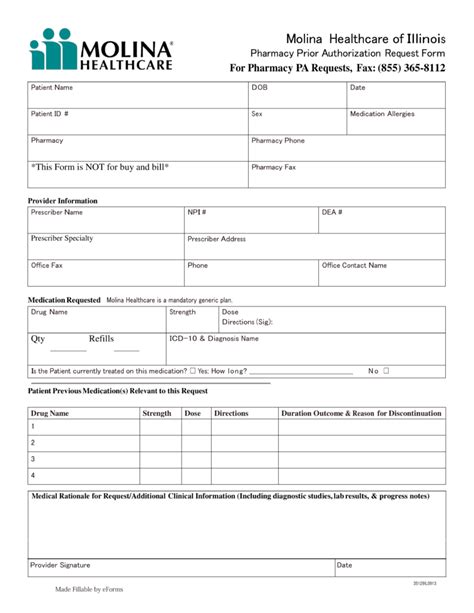
The Molina prior authorization form is a tool used by healthcare providers to request approval for medications and treatments from Molina Healthcare. This form is designed to simplify the prior authorization process, making it easier for healthcare providers to request approval and for Molina Healthcare to review and make determinations.
How to Complete the Molina Prior Authorization Form
Completing the Molina prior authorization form requires careful attention to detail and accurate information. Here are the steps to follow:
- Gather necessary information: Before starting the form, gather all necessary information, including the patient's name, date of birth, insurance information, and medication details.
- Complete the patient information section: Fill in the patient's name, date of birth, and insurance information.
- Complete the medication information section: Fill in the medication name, dosage, and frequency.
- Complete the clinical information section: Provide clinical information to support the request, including diagnosis, medical history, and treatment plan.
- Sign and date the form: Sign and date the form to certify that the information is accurate and complete.
Submission and Review Process

Once the Molina prior authorization form is complete, it can be submitted to Molina Healthcare for review. The submission and review process typically involves the following steps:
- Submission: Submit the completed form to Molina Healthcare via fax, email, or online portal.
- Review: Molina Healthcare reviews the request to determine whether the medication or treatment is medically necessary and covered under the patient's insurance plan.
- Determination: Molina Healthcare makes a determination and notifies the healthcare provider of the outcome.
What to Expect After Submission
After submitting the Molina prior authorization form, healthcare providers can expect to receive a determination from Molina Healthcare. If the request is approved, the patient can proceed with the prescribed medication or treatment. If the request is denied, the healthcare provider can appeal the decision or explore alternative treatment options.
Conclusion: Simplifying Prior Authorization with Molina

The Molina prior authorization form has simplified the process of obtaining approval for medications and treatments. By providing a streamlined and efficient process, healthcare providers can focus on delivering quality patient care while minimizing administrative burdens. Patients can rest assured that they are receiving safe and effective treatments, and insurance companies can trust that the process is fair and transparent.
Take Action:
- Download the Molina prior authorization form today and start simplifying the prior authorization process.
- Contact Molina Healthcare to learn more about their prior authorization process and requirements.
- Share your experiences with the Molina prior authorization form and help others navigate the process.
By working together, we can make the prior authorization process more efficient and effective, ultimately improving patient outcomes and reducing healthcare costs.
What is prior authorization?
+Prior authorization is a process used by insurance companies to determine whether a specific medication or treatment is medically necessary and covered under a patient's insurance plan.
How do I complete the Molina prior authorization form?
+To complete the Molina prior authorization form, gather necessary information, complete the patient information section, medication information section, and clinical information section, and sign and date the form.
What happens after I submit the Molina prior authorization form?
+After submitting the Molina prior authorization form, Molina Healthcare reviews the request and makes a determination. If the request is approved, the patient can proceed with the prescribed medication or treatment. If the request is denied, the healthcare provider can appeal the decision or explore alternative treatment options.