Missouri's Medicaid program, MO HealthNet, serves over 1 million low-income individuals and families across the state. One crucial aspect of this program is prior authorization, which allows healthcare providers to request pre-approval for certain medical treatments, medications, and services. However, the prior authorization process can be complex and time-consuming, leading to delays in patient care. In this article, we will explore five ways to simplify MO HealthNet prior authorization, making it more efficient for healthcare providers and ensuring better patient outcomes.
Understanding MO HealthNet Prior Authorization

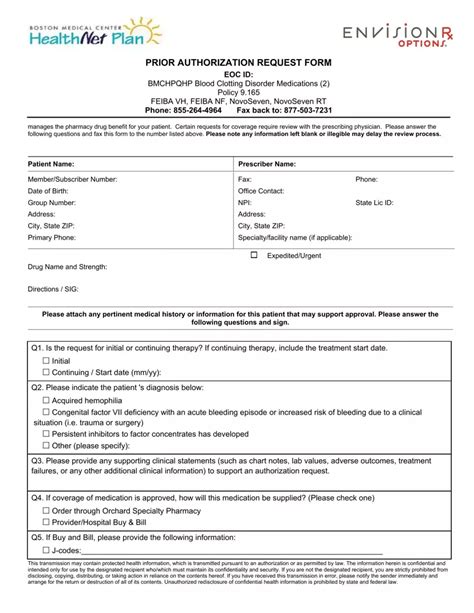
Prior authorization is a critical component of MO HealthNet, aimed at ensuring that patients receive necessary and cost-effective care. The process involves healthcare providers submitting requests to MO HealthNet for pre-approval of certain medical services, which are then reviewed and approved or denied based on the program's guidelines. While prior authorization helps to prevent unnecessary costs and ensure patient safety, it can also lead to administrative burdens and delays in care.
Benefits of Streamlining Prior Authorization
Simplifying the prior authorization process can have numerous benefits for both healthcare providers and patients. Some of the key advantages include:
- Reduced administrative burdens: By streamlining the prior authorization process, healthcare providers can spend less time on paperwork and more time on patient care.
- Improved patient outcomes: Efficient prior authorization can lead to faster access to necessary treatments, resulting in better patient outcomes and improved quality of life.
- Enhanced provider satisfaction: Simplifying prior authorization can reduce frustration and burnout among healthcare providers, leading to improved job satisfaction and reduced turnover rates.
5 Ways to Simplify MO HealthNet Prior Authorization

- Implement Electronic Prior Authorization
Switching from paper-based to electronic prior authorization can significantly simplify the process. Electronic prior authorization systems can automate workflows, reduce errors, and provide real-time updates on the status of requests. MO HealthNet can consider implementing electronic prior authorization systems that integrate with healthcare providers' electronic health records (EHRs) and practice management systems.
Advantages of Electronic Prior Authorization
- Increased efficiency: Electronic prior authorization can reduce processing times and minimize the need for manual data entry.
- Improved accuracy: Electronic systems can automatically check for errors and inconsistencies, reducing the risk of denied requests.
- Enhanced transparency: Electronic prior authorization systems can provide real-time updates on the status of requests, keeping healthcare providers informed.
- Develop Clear Guidelines and Criteria
MO HealthNet can simplify prior authorization by developing clear guidelines and criteria for healthcare providers. This can include:
- Establishing clear criteria for prior authorization: MO HealthNet can create specific guidelines outlining the requirements for prior authorization, reducing confusion and uncertainty among healthcare providers.
- Providing detailed instructions: MO HealthNet can offer step-by-step instructions on the prior authorization process, including required documentation and submission procedures.
- Creating a provider portal: MO HealthNet can develop a dedicated portal for healthcare providers, providing access to prior authorization guidelines, forms, and tracking information.
Benefits of Clear Guidelines and Criteria
- Reduced errors: Clear guidelines can minimize errors and inconsistencies in prior authorization requests.
- Improved provider satisfaction: Transparent guidelines can reduce frustration and confusion among healthcare providers, leading to improved job satisfaction.
- Enhanced patient outcomes: Clear guidelines can ensure that patients receive necessary treatments in a timely manner, resulting in better patient outcomes.
- Implement a Prior Authorization Portal
MO HealthNet can simplify prior authorization by implementing a dedicated portal for healthcare providers. This portal can provide:
- Online submission and tracking: Healthcare providers can submit prior authorization requests and track the status of their requests in real-time.
- Automated workflows: The portal can automate workflows, reducing the need for manual data entry and minimizing errors.
- Access to prior authorization guidelines: The portal can provide access to clear guidelines and criteria for prior authorization, reducing confusion and uncertainty among healthcare providers.
Advantages of a Prior Authorization Portal
- Increased efficiency: A prior authorization portal can reduce processing times and minimize the need for manual data entry.
- Improved transparency: The portal can provide real-time updates on the status of requests, keeping healthcare providers informed.
- Enhanced provider satisfaction: A user-friendly portal can reduce frustration and burnout among healthcare providers, leading to improved job satisfaction.
- Reduce Prior Authorization Requirements
MO HealthNet can simplify prior authorization by reducing the number of requirements for healthcare providers. This can include:
- Eliminating unnecessary paperwork: MO HealthNet can identify and eliminate unnecessary paperwork and documentation requirements, reducing the administrative burden on healthcare providers.
- Streamlining prior authorization forms: MO HealthNet can simplify prior authorization forms, making it easier for healthcare providers to complete and submit requests.
- Implementing pre-authorization lists: MO HealthNet can create pre-authorization lists for commonly prescribed medications and treatments, reducing the need for individual prior authorization requests.
Benefits of Reducing Prior Authorization Requirements
- Reduced administrative burdens: Reducing prior authorization requirements can minimize the administrative burden on healthcare providers, allowing them to focus on patient care.
- Improved patient outcomes: Streamlined prior authorization can lead to faster access to necessary treatments, resulting in better patient outcomes and improved quality of life.
- Enhanced provider satisfaction: Simplifying prior authorization can reduce frustration and burnout among healthcare providers, leading to improved job satisfaction and reduced turnover rates.
- Monitor and Evaluate Prior Authorization Processes
MO HealthNet can simplify prior authorization by monitoring and evaluating the process regularly. This can include:
- Tracking key performance indicators (KPIs): MO HealthNet can track KPIs such as processing times, denial rates, and provider satisfaction, identifying areas for improvement.
- Conducting provider surveys: MO HealthNet can conduct regular surveys among healthcare providers to gather feedback and identify areas for improvement.
- Implementing changes based on feedback: MO HealthNet can implement changes to the prior authorization process based on feedback from healthcare providers, ensuring that the process is efficient and effective.
Benefits of Monitoring and Evaluating Prior Authorization Processes
- Improved efficiency: Regular monitoring and evaluation can identify areas for improvement, allowing MO HealthNet to streamline the prior authorization process.
- Enhanced provider satisfaction: Gathering feedback from healthcare providers can help MO HealthNet identify and address areas of concern, leading to improved job satisfaction and reduced turnover rates.
- Better patient outcomes: Efficient prior authorization can lead to faster access to necessary treatments, resulting in better patient outcomes and improved quality of life.
Conclusion: Simplifying MO HealthNet Prior Authorization

Simplifying MO HealthNet prior authorization is crucial for ensuring that patients receive necessary treatments in a timely manner. By implementing electronic prior authorization, developing clear guidelines and criteria, implementing a prior authorization portal, reducing prior authorization requirements, and monitoring and evaluating prior authorization processes, MO HealthNet can simplify the prior authorization process, reducing administrative burdens and improving patient outcomes.
We encourage healthcare providers and patients to share their experiences and suggestions for simplifying MO HealthNet prior authorization. By working together, we can create a more efficient and effective prior authorization process that benefits everyone involved.
What is MO HealthNet prior authorization?
+MO HealthNet prior authorization is a process that allows healthcare providers to request pre-approval for certain medical treatments, medications, and services.
Why is prior authorization necessary?
+Prior authorization helps to prevent unnecessary costs and ensure patient safety by ensuring that patients receive necessary and cost-effective care.
How can I simplify the prior authorization process?
+MO HealthNet can simplify the prior authorization process by implementing electronic prior authorization, developing clear guidelines and criteria, implementing a prior authorization portal, reducing prior authorization requirements, and monitoring and evaluating prior authorization processes.