Illinois healthcare providers often encounter various administrative tasks when working with insurance companies. One such task is completing prior authorization forms, which can be time-consuming and may delay patient care. In this article, we will focus on the Meridian Illinois Prior Authorization Form, providing a step-by-step guide on how to file it correctly.
Understanding Prior Authorization
Prior authorization, also known as pre-authorization or pre-certification, is the process by which healthcare providers obtain approval from a patient's insurance company before providing specific treatments or services. This process is designed to ensure that patients receive necessary and cost-effective care. However, it can be a source of frustration for both providers and patients due to the paperwork and potential delays involved.

Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It helps ensure that patients receive medically necessary treatments.
- It prevents unnecessary or costly procedures.
- It streamlines the healthcare process by reducing administrative burdens.
However, prior authorization can be a complex and time-consuming process, often requiring multiple phone calls, faxes, and paperwork. This can lead to delays in patient care and increased frustration for healthcare providers.
Common Challenges with Prior Authorization
Some common challenges associated with prior authorization include:
- Lengthy processing times
- Lack of standardization in forms and procedures
- Inadequate communication between providers and insurance companies
- Increased administrative burdens on healthcare staff
To address these challenges, it's essential to understand the specific requirements for each insurance company and to have a streamlined process in place for completing prior authorization forms.
Meridian Illinois Prior Authorization Form: A Step-by-Step Guide
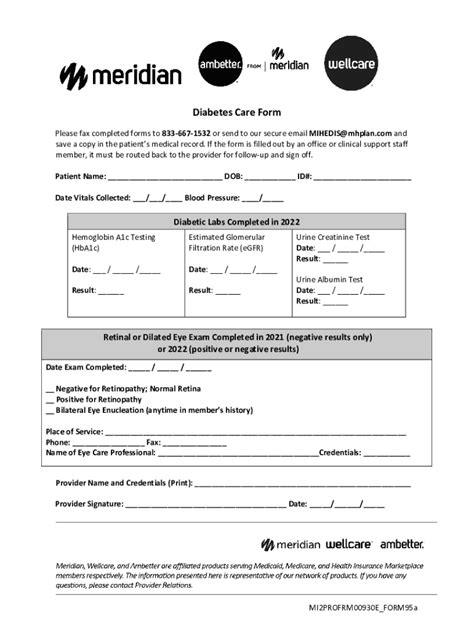
The Meridian Illinois Prior Authorization Form is a specific document required by Meridian Health Plan of Illinois for certain treatments or services. Here's a step-by-step guide to help you file the form correctly:

- Determine if Prior Authorization is Required: Check the Meridian Health Plan of Illinois coverage policies to determine if prior authorization is required for the specific treatment or service.
- Gather Necessary Information: Collect all relevant patient information, including medical history, current diagnosis, and treatment plans.
- Complete the Prior Authorization Form: Fill out the Meridian Illinois Prior Authorization Form accurately and completely, ensuring that all required fields are filled in.
- Attach Supporting Documentation: Include any supporting documentation, such as medical records or test results, to justify the requested treatment or service.
- Submit the Form: Fax or mail the completed form to Meridian Health Plan of Illinois, following their specific submission guidelines.
Best Practices for Filing Prior Authorization Forms
To streamline the prior authorization process and reduce potential delays, follow these best practices:
- Verify Patient Eligibility: Confirm patient eligibility and coverage before submitting the prior authorization form.
- Use Standardized Forms: Use standardized prior authorization forms to reduce errors and increase efficiency.
- Provide Complete Information: Ensure that all required fields are filled in accurately and completely to avoid delays or denials.
- Follow Up: Follow up with Meridian Health Plan of Illinois to confirm receipt of the prior authorization form and to address any potential issues.
Electronic Prior Authorization: A More Efficient Solution
Electronic prior authorization (ePA) is a digital solution that streamlines the prior authorization process, reducing paperwork and increasing efficiency. ePA systems allow healthcare providers to submit prior authorization requests electronically, receiving instant feedback and reducing the risk of errors or delays.

Benefits of Electronic Prior Authorization
The benefits of electronic prior authorization include:
- Increased Efficiency: ePA systems reduce paperwork and increase the speed of prior authorization requests.
- Improved Accuracy: Electronic systems reduce the risk of errors or incomplete information.
- Enhanced Patient Care: ePA systems enable healthcare providers to focus on patient care, rather than administrative tasks.
By adopting electronic prior authorization, healthcare providers can improve the efficiency and effectiveness of the prior authorization process, ultimately enhancing patient care and outcomes.
Conclusion
Completing prior authorization forms, such as the Meridian Illinois Prior Authorization Form, can be a complex and time-consuming process. However, by following the step-by-step guide outlined in this article and adopting best practices, healthcare providers can streamline the process and reduce potential delays. Additionally, electronic prior authorization offers a more efficient solution, enabling healthcare providers to focus on patient care while improving the overall efficiency of the prior authorization process.
We encourage you to share your experiences with prior authorization forms in the comments section below. If you have any questions or would like to learn more about electronic prior authorization, please don't hesitate to ask.
What is prior authorization?
+Prior authorization, also known as pre-authorization or pre-certification, is the process by which healthcare providers obtain approval from a patient's insurance company before providing specific treatments or services.
Why is prior authorization important?
+Prior authorization is essential for ensuring that patients receive medically necessary treatments, preventing unnecessary or costly procedures, and streamlining the healthcare process by reducing administrative burdens.
What are the benefits of electronic prior authorization?
+The benefits of electronic prior authorization include increased efficiency, improved accuracy, and enhanced patient care.