The medical billing process can be complex and time-consuming, especially when it comes to prior authorization. The Medimpact prior authorization form is an essential document that healthcare providers need to complete to ensure that their patients receive the necessary medical treatments. In this article, we will guide you through the 5 easy steps to complete the Medimpact prior authorization form.
Understanding the Importance of Prior Authorization

Prior authorization is a process that healthcare providers must follow to obtain approval from insurance companies before administering certain medical treatments or procedures. This process ensures that the treatment is medically necessary and meets the insurance company's guidelines. The Medimpact prior authorization form is a standardized document that healthcare providers can use to request prior authorization from insurance companies.
Why is Prior Authorization Important?
Prior authorization is crucial because it:
- Ensures that patients receive medically necessary treatments
- Reduces the risk of denied claims
- Saves time and resources for healthcare providers
- Helps insurance companies manage healthcare costs
Step 1: Gather Required Information

To complete the Medimpact prior authorization form, healthcare providers need to gather the required information. This includes:
- Patient demographics and insurance information
- Medical history and current diagnosis
- Treatment or procedure details
- Supporting documentation (e.g., medical records, test results)
Tips for Gathering Information
- Ensure that all patient information is accurate and up-to-date
- Verify insurance coverage and benefits
- Review medical history and current diagnosis to ensure that the treatment is medically necessary
- Gather all supporting documentation to avoid delays in the prior authorization process
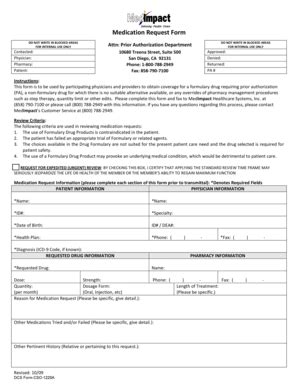
Step 2: Complete the Medimpact Prior Authorization Form

Once the required information is gathered, healthcare providers can complete the Medimpact prior authorization form. The form typically includes sections for:
- Patient information
- Medical history and current diagnosis
- Treatment or procedure details
- Supporting documentation
Tips for Completing the Form
- Ensure that all sections are completed accurately and thoroughly
- Use clear and concise language when describing the medical condition and treatment
- Attach all supporting documentation to the form
- Review the form for errors or omissions before submitting
Step 3: Submit the Form for Review

Once the Medimpact prior authorization form is complete, healthcare providers can submit it for review. The form can be submitted electronically or by mail, depending on the insurance company's requirements.
Tips for Submitting the Form
- Ensure that the form is submitted on time to avoid delays in the prior authorization process
- Verify that the form is complete and accurate before submitting
- Keep a record of the submission, including the date and time
Step 4: Follow Up on the Prior Authorization Request

After submitting the Medimpact prior authorization form, healthcare providers should follow up on the prior authorization request. This includes:
- Checking the status of the request
- Responding to additional requests for information
- Reviewing the insurance company's decision
Tips for Following Up
- Follow up on the request within 2-3 business days of submitting the form
- Be prepared to provide additional information or documentation
- Review the insurance company's decision and appeal if necessary
Step 5: Receive and Review the Prior Authorization Decision

Once the prior authorization request is reviewed, healthcare providers will receive a decision from the insurance company. The decision may be:
- Approved: The treatment or procedure is approved, and the patient can receive the necessary care.
- Denied: The treatment or procedure is denied, and the patient may need to appeal the decision.
- Partially approved: The treatment or procedure is partially approved, and the patient may need to provide additional information or documentation.
Tips for Receiving and Reviewing the Decision
- Review the decision carefully to ensure that it is accurate and complete
- Understand the reasons for denial or partial approval
- Appeal the decision if necessary
By following these 5 easy steps, healthcare providers can complete the Medimpact prior authorization form and ensure that their patients receive the necessary medical treatments. Remember to gather required information, complete the form accurately, submit the form for review, follow up on the request, and receive and review the prior authorization decision.
What is the purpose of the Medimpact prior authorization form?
+The Medimpact prior authorization form is used to request prior authorization from insurance companies for certain medical treatments or procedures.
How long does the prior authorization process take?
+The prior authorization process typically takes 2-5 business days, but may vary depending on the insurance company and the complexity of the request.
Can I appeal a denied prior authorization decision?
+Yes, you can appeal a denied prior authorization decision. You should review the reasons for denial and provide additional information or documentation to support your appeal.
We hope this article has been helpful in guiding you through the 5 easy steps for completing the Medimpact prior authorization form. If you have any further questions or concerns, please don't hesitate to comment below. Share this article with your colleagues and friends who may find it useful.