As a healthcare provider or patient, navigating the complexities of prior authorization can be a daunting task. IU Health, a prominent healthcare system, requires prior authorization for certain medical services and treatments. In this article, we will break down the IU Health Prior Authorization Form into 5 easy steps, making it more manageable and efficient for healthcare professionals and patients alike.

Understanding Prior Authorization
Prior authorization is a process used by healthcare providers and insurance companies to determine the medical necessity of a treatment or service before it is rendered. This process helps ensure that patients receive the most effective and cost-efficient care. IU Health requires prior authorization for certain medical services, including prescription medications, surgical procedures, and diagnostic tests.
Why is Prior Authorization Important?
Prior authorization is crucial for several reasons:
- Ensures medical necessity: Prior authorization ensures that the requested treatment or service is medically necessary and aligns with established clinical guidelines.
- Reduces unnecessary costs: By reviewing requests before treatment, prior authorization helps reduce unnecessary healthcare costs and ensures that patients receive the most cost-effective care.
- Improves patient outcomes: Prior authorization promotes the use of evidence-based treatments, leading to better patient outcomes and improved quality of life.
Step 1: Determine if Prior Authorization is Required
Before starting the prior authorization process, it's essential to determine if it's required for the specific medical service or treatment. IU Health provides a list of services that require prior authorization on their website. Healthcare providers can also contact IU Health's prior authorization department to confirm whether prior authorization is necessary.

What Services Require Prior Authorization?
IU Health requires prior authorization for various medical services, including:
- Prescription medications (e.g., specialty medications, injectables)
- Surgical procedures (e.g., elective surgeries, transplants)
- Diagnostic tests (e.g., MRI, CT scans)
- Durable medical equipment (e.g., wheelchairs, oxygen therapy)
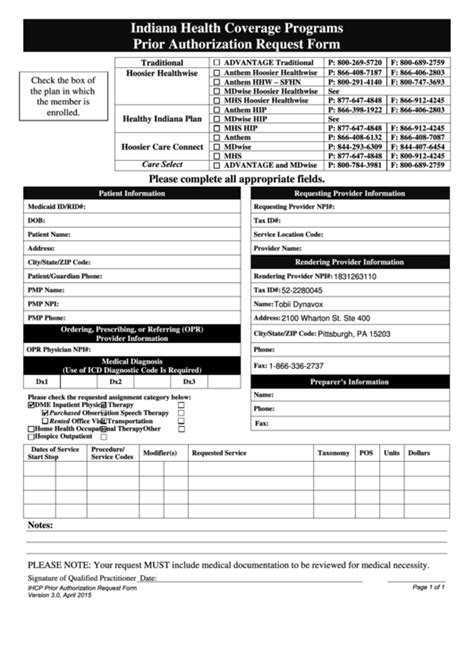
Step 2: Gather Required Information
To initiate the prior authorization process, healthcare providers must gather the necessary information, including:
- Patient demographics and insurance information
- Treatment or service details (e.g., medication name, dosage, frequency)
- Medical records and supporting documentation (e.g., lab results, medical history)

What Information is Required for Prior Authorization?
IU Health requires the following information for prior authorization:
- Patient's name, date of birth, and insurance information
- Treatment or service details, including medication name, dosage, and frequency
- Medical records and supporting documentation, such as lab results and medical history
Step 3: Submit the Prior Authorization Request
Once the required information is gathered, healthcare providers can submit the prior authorization request to IU Health. This can be done via phone, fax, or online portal.

How to Submit a Prior Authorization Request
IU Health accepts prior authorization requests via:
- Phone: (phone number)
- Fax: (fax number)
- Online portal: (online portal URL)
Step 4: Review and Respond to the Prior Authorization Decision
After submitting the prior authorization request, IU Health will review the information and make a determination. Healthcare providers will receive a notification of the decision, which may include:
- Approval: The requested treatment or service is approved.
- Denial: The requested treatment or service is denied.
- Additional information requested: IU Health requires additional information to make a determination.

What to Do if Prior Authorization is Denied
If prior authorization is denied, healthcare providers can:
- Appeal the decision
- Provide additional information to support the request
- Consider alternative treatments or services
Step 5: Follow Up and Verify Prior Authorization
Once the prior authorization decision is made, healthcare providers should follow up to verify the status and ensure that the patient receives the approved treatment or service.

Why is Follow-Up Important?
Follow-up is crucial to ensure that:
- The patient receives the approved treatment or service
- Any additional requirements or documentation are completed
- The prior authorization is updated in the patient's record
By following these 5 easy steps, healthcare providers and patients can navigate the IU Health Prior Authorization Form process with ease, ensuring that patients receive the necessary medical treatments and services in a timely and efficient manner.
We invite you to share your experiences or ask questions about the prior authorization process in the comments below.