Navigating the complex world of healthcare insurance can be overwhelming, especially when it comes to ensuring that you receive the necessary care without breaking the bank. One crucial aspect of this process is obtaining pre-certification, also known as prior authorization, for medical procedures and treatments. In this article, we will delve into the HMSA precertification form, providing a step-by-step guide on how to navigate this process seamlessly.
Understanding the Importance of Precertification
Precertification is a process used by health insurance companies to determine whether a specific medical procedure or treatment is medically necessary and covered under your policy. This process helps prevent unnecessary medical expenses and ensures that you receive the necessary care without financial burdens. HMSA, a leading health insurance provider, requires precertification for various medical services, including hospital stays, surgeries, and other specialized treatments.

Benefits of Precertification
The precertification process offers several benefits to both patients and healthcare providers. Some of the key advantages include:
- Reduced medical costs: By verifying the medical necessity of a procedure, precertification helps prevent unnecessary expenses.
- Improved quality of care: Precertification ensures that patients receive the most appropriate treatment for their condition.
- Enhanced patient safety: By verifying the credentials of healthcare providers, precertification promotes safe and effective care.
Understanding the HMSA Precertification Form
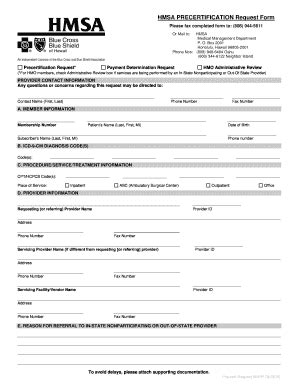
The HMSA precertification form is a document that patients or their healthcare providers must complete to request prior authorization for a medical procedure or treatment. The form typically requires information about the patient, the proposed treatment, and the healthcare provider.

Key Components of the HMSA Precertification Form
The HMSA precertification form typically includes the following key components:
- Patient information: This section requires the patient's name, date of birth, and HMSA membership number.
- Procedure information: This section requires details about the proposed medical procedure or treatment, including the date and location of the procedure.
- Healthcare provider information: This section requires information about the healthcare provider, including their name, address, and contact details.
Step-by-Step Guide to Completing the HMSA Precertification Form
To ensure a smooth precertification process, follow these steps:
- Gather necessary information: Collect all required information, including patient details, procedure information, and healthcare provider details.
- Download the precertification form: Obtain the HMSA precertification form from the HMSA website or by contacting their customer service department.
- Complete the form: Fill out the form accurately and thoroughly, ensuring that all required information is provided.
- Submit the form: Submit the completed form to HMSA via fax, email, or online portal.
- Wait for review: Allow HMSA time to review the precertification request.
- Receive approval or denial: HMSA will notify you of their decision, either approving or denying the precertification request.

Tips for a Smooth Precertification Process
To ensure a seamless precertification process, keep the following tips in mind:
- Plan ahead: Submit the precertification form well in advance of the proposed procedure date.
- Provide complete information: Ensure that all required information is provided to avoid delays or denials.
- Follow up: If you haven't received a response from HMSA, follow up to confirm the status of your precertification request.
Common Mistakes to Avoid
To avoid delays or denials, be aware of the following common mistakes:
- Incomplete information: Failing to provide all required information can lead to delays or denials.
- Inaccurate information: Providing inaccurate information can result in denials or delays.
- Insufficient time: Submitting the precertification form too close to the proposed procedure date can lead to delays or denials.

Conclusion
Navigating the HMSA precertification form process can seem daunting, but by following the step-by-step guide and tips outlined in this article, you can ensure a smooth and efficient experience. Remember to plan ahead, provide complete information, and follow up on your precertification request to avoid delays or denials. By taking these steps, you can ensure that you receive the necessary medical care without financial burdens.

We hope this article has provided valuable insights into the HMSA precertification form process. If you have any further questions or concerns, please don't hesitate to comment below or share this article with others who may benefit from this information.
What is precertification?
+Precertification is a process used by health insurance companies to determine whether a specific medical procedure or treatment is medically necessary and covered under your policy.
What is the purpose of the HMSA precertification form?
+The HMSA precertification form is used to request prior authorization for a medical procedure or treatment, ensuring that the treatment is medically necessary and covered under your policy.
How long does the precertification process take?
+The precertification process typically takes a few days to a week, depending on the complexity of the request and the speed of the healthcare provider and HMSA.