Prior authorization (prior auth) is a crucial process in the healthcare industry that ensures patients receive necessary medical treatments while minimizing costs and promoting safe and effective care. Highmark, one of the largest health insurance companies in the United States, requires prior authorization for certain medical procedures and treatments. If you're a healthcare provider or patient, understanding the Highmark prior auth form and process is essential. In this article, we'll provide an easy step-by-step guide to help you navigate the Highmark prior auth form and ensure a smooth authorization process.
What is Prior Authorization (Prior Auth)?
Prior authorization is a process used by health insurance companies to review and approve certain medical treatments, procedures, or prescriptions before they are administered or dispensed. This process ensures that patients receive necessary and cost-effective care while minimizing unnecessary expenses. Prior auth also helps prevent medication errors and promotes safe and effective treatment.

Why is Prior Authorization Required?
Prior authorization is required for several reasons:
- To ensure that patients receive medically necessary and cost-effective care
- To prevent medication errors and promote safe and effective treatment
- To minimize unnecessary expenses and reduce healthcare costs
- To comply with regulatory requirements and industry standards
Highmark Prior Auth Form: What You Need to Know
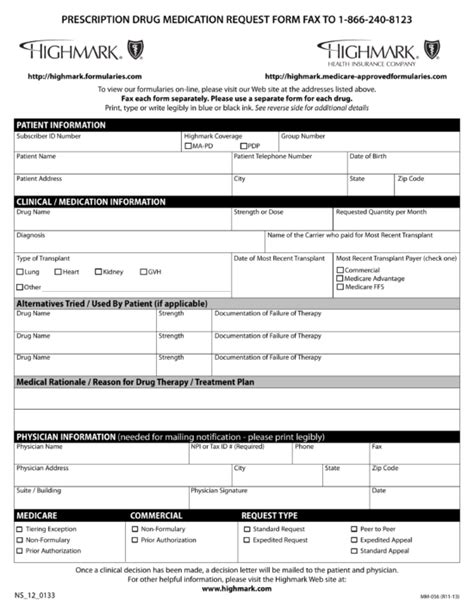
The Highmark prior auth form is a document used by healthcare providers to request prior authorization for certain medical treatments or procedures. The form requires providers to submit patient information, medical history, and treatment details to Highmark for review and approval.

Required Information
To complete the Highmark prior auth form, providers must submit the following information:
- Patient demographics and insurance information
- Medical history and diagnosis
- Treatment details, including medication, dosage, and duration
- Clinical documentation and supporting medical records
Step-by-Step Guide to Completing the Highmark Prior Auth Form
Here's a step-by-step guide to help you complete the Highmark prior auth form:
- Gather patient information: Collect patient demographics, insurance information, and medical history.
- Determine the required treatment: Identify the medical treatment or procedure that requires prior authorization.
- Complete the prior auth form: Fill out the Highmark prior auth form, ensuring that all required information is included.
- Attach supporting documentation: Include clinical documentation and supporting medical records to support the prior auth request.
- Submit the prior auth request: Fax or submit the prior auth request to Highmark for review and approval.

Highmark Prior Auth Status: How to Check
Once you've submitted the prior auth request, you can check the status online or by phone. Here's how:
- Online: Visit the Highmark website and log in to your account to check the prior auth status.
- Phone: Call Highmark's prior auth hotline to check the status of your request.
Tips for a Smooth Prior Auth Process
Here are some tips to ensure a smooth prior auth process:
- Complete the prior auth form accurately: Ensure that all required information is included to avoid delays or denials.
- Attach supporting documentation: Include clinical documentation and supporting medical records to support the prior auth request.
- Submit the prior auth request timely: Submit the prior auth request in a timely manner to avoid delays in treatment.

Conclusion
The Highmark prior auth form is a crucial document that ensures patients receive necessary and cost-effective care. By following the step-by-step guide outlined in this article, healthcare providers can ensure a smooth prior auth process and minimize delays in treatment. Remember to complete the prior auth form accurately, attach supporting documentation, and submit the request in a timely manner.
Encourage Engagement
We hope this article has provided valuable insights into the Highmark prior auth form and process. If you have any questions or comments, please feel free to share them below. Don't forget to share this article with your colleagues and friends who may find it helpful.
What is prior authorization?
+Prior authorization is a process used by health insurance companies to review and approve certain medical treatments, procedures, or prescriptions before they are administered or dispensed.
Why is prior authorization required?
+Prior authorization is required to ensure that patients receive medically necessary and cost-effective care, prevent medication errors, and minimize unnecessary expenses.
How do I check the status of my prior auth request?
+You can check the status of your prior auth request online or by phone. Visit the Highmark website and log in to your account to check the prior auth status, or call Highmark's prior auth hotline.