As a healthcare provider, obtaining prior authorization for medical treatments and services is a crucial step in ensuring that your patients receive the care they need while also minimizing the risk of denied claims and delayed payments. One of the most widely used authorization forms in the healthcare industry is the Healthnet Authorization Form. In this article, we will provide a step-by-step guide on how to complete the Healthnet Authorization Form, highlighting the key information required and the benefits of using this form.

Why is Prior Authorization Important?
Prior authorization, also known as pre-certification or pre-authorization, is the process of obtaining approval from a health insurance company before providing medical treatment or services to a patient. This process helps to ensure that the treatment or service is medically necessary and meets the insurance company's coverage criteria. By obtaining prior authorization, healthcare providers can avoid denied claims and delayed payments, which can negatively impact their cash flow and reputation.
What is the Healthnet Authorization Form?
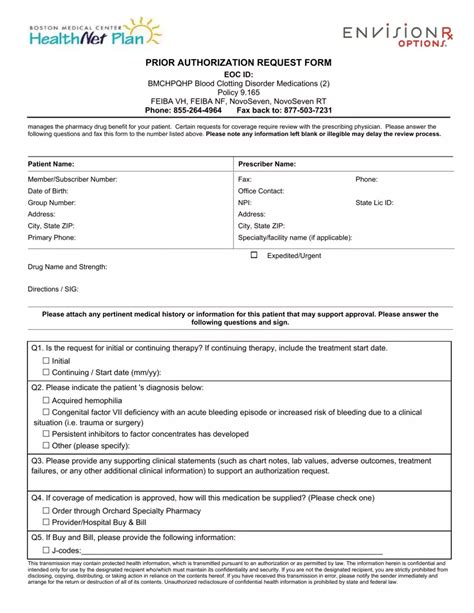
The Healthnet Authorization Form is a standardized form used by healthcare providers to request prior authorization for medical treatments and services from Healthnet, a leading health insurance company. The form is designed to collect all the necessary information required by Healthnet to make an informed decision about the authorization request. The form is typically completed by the healthcare provider or their staff and submitted to Healthnet for review and approval.
Step-By-Step Guide to Completing the Healthnet Authorization Form
Completing the Healthnet Authorization Form requires careful attention to detail and accurate information. Here is a step-by-step guide to help you complete the form correctly:
Step 1: Patient Information
The first section of the form requires patient information, including:
- Patient name and date of birth
- Healthnet ID number
- Contact information (address, phone number, and email)

Step 2: Treatment or Service Information
The next section requires information about the treatment or service being requested, including:
- Description of the treatment or service
- CPT code(s) and modifier(s)
- Date of service or treatment start date
- Number of sessions or units requested
Treatment or Service Information Requirements
- Be specific when describing the treatment or service.
- Use the correct CPT code(s) and modifier(s) to ensure accurate reimbursement.
- Include the date of service or treatment start date to avoid delays.
Step 3: Clinical Information
The clinical information section requires documentation of the patient's medical condition, including:
- Diagnosis code(s) and description
- Medical history and relevant test results
- Treatment plan and goals

Step 4: Supporting Documentation
The final section requires supporting documentation, including:
- Medical records and test results
- Treatment plans and progress notes
- Correspondence with other healthcare providers
Supporting Documentation Requirements
- Include all relevant medical records and test results.
- Ensure that treatment plans and progress notes are up-to-date and accurate.
- Attach correspondence with other healthcare providers, if applicable.
Step 5: Submission
Once the form is complete, submit it to Healthnet for review and approval. Ensure that all required documentation is attached and that the form is signed and dated.
Benefits of Using the Healthnet Authorization Form
Using the Healthnet Authorization Form provides several benefits, including:
- Streamlined prior authorization process
- Reduced risk of denied claims and delayed payments
- Improved patient care and outcomes
- Enhanced communication between healthcare providers and Healthnet

Conclusion
The Healthnet Authorization Form is a crucial tool for healthcare providers to obtain prior authorization for medical treatments and services. By following the step-by-step guide outlined in this article, healthcare providers can ensure that the form is completed accurately and efficiently, reducing the risk of denied claims and delayed payments. Remember to attach all required documentation and submit the form to Healthnet for review and approval.
We hope that this article has provided you with a comprehensive understanding of the Healthnet Authorization Form and its importance in the healthcare industry. If you have any questions or concerns, please feel free to comment below or share this article with your colleagues.
What is the purpose of the Healthnet Authorization Form?
+The Healthnet Authorization Form is used to request prior authorization for medical treatments and services from Healthnet.
Who completes the Healthnet Authorization Form?
+The Healthnet Authorization Form is typically completed by the healthcare provider or their staff.
What information is required on the Healthnet Authorization Form?
+The form requires patient information, treatment or service information, clinical information, and supporting documentation.