The healthcare system can be complex and overwhelming, especially when it comes to managing medications and navigating insurance coverage. One crucial aspect of this process is the prior authorization form, which helps ensure that patients receive the necessary medications while also controlling costs and promoting safe prescribing practices. In this article, we will delve into the Healthfirst Medication Prior Authorization Form, providing a step-by-step guide to help healthcare providers, patients, and caregivers understand the process.
Understanding the Importance of Prior Authorization
Prior authorization is a process used by health insurance companies to determine whether a particular medication or treatment is medically necessary and covered under the patient's insurance plan. This process helps prevent unnecessary prescriptions, reduces healthcare costs, and promotes the use of evidence-based treatments. For patients, prior authorization can ensure that they receive the most effective and safest medications for their condition, while also minimizing out-of-pocket expenses.

The Healthfirst Medication Prior Authorization Form: An Overview
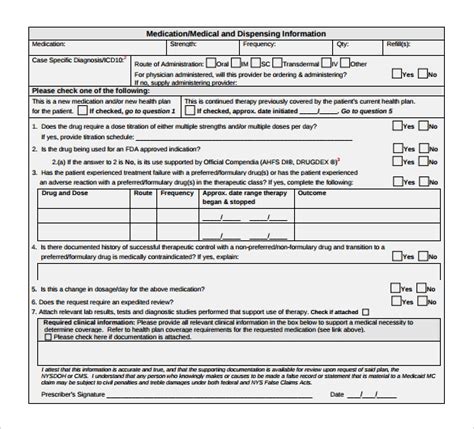
The Healthfirst Medication Prior Authorization Form is a specific document used by healthcare providers to request prior authorization for medications that are not covered under the patient's insurance plan or require additional approval. The form typically includes information about the patient, the prescribed medication, and the medical condition being treated.

Step 1: Gather Required Information
Before completing the Healthfirst Medication Prior Authorization Form, healthcare providers must gather the necessary information, including:
- Patient demographics and insurance information
- Prescription details, including the medication name, dosage, and frequency
- Medical condition being treated and relevant medical history
- Relevant laboratory results or diagnostic tests
Completing the Healthfirst Medication Prior Authorization Form
Once the required information is gathered, healthcare providers can complete the Healthfirst Medication Prior Authorization Form. The form typically includes the following sections:
Section 1: Patient Information
- Patient name and date of birth
- Insurance information, including policy number and group number
- Contact information, including phone number and email
Section 2: Prescription Information
- Medication name and dosage
- Frequency and duration of treatment
- Prescriber information, including name and contact information
Section 3: Medical Condition and History
- Description of the medical condition being treated
- Relevant medical history, including previous treatments and allergies
- Laboratory results or diagnostic tests supporting the treatment plan

Submitting the Healthfirst Medication Prior Authorization Form
Once the form is completed, healthcare providers can submit it to Healthfirst for review. The submission process typically involves:
- Faxing or mailing the completed form to Healthfirst
- Providing additional supporting documentation, such as medical records or laboratory results
- Following up with Healthfirst to confirm receipt and review status
Timeline for Prior Authorization Review
Healthfirst typically reviews prior authorization requests within 24-48 hours. However, the review process may take longer if additional information is required or if the request is submitted during peak periods.
Appealing a Prior Authorization Denial
If a prior authorization request is denied, healthcare providers can appeal the decision by submitting additional information or supporting documentation. The appeal process typically involves:
- Reviewing the denial letter and identifying the reasons for denial
- Gathering additional information or supporting documentation to address the denial reasons
- Submitting the appeal request to Healthfirst, including the additional information or supporting documentation

Conclusion: Navigating the Healthfirst Medication Prior Authorization Form
The Healthfirst Medication Prior Authorization Form is an essential tool for healthcare providers, patients, and caregivers to ensure that necessary medications are approved and covered under the patient's insurance plan. By understanding the importance of prior authorization and following the step-by-step guide outlined in this article, healthcare providers can efficiently navigate the process and provide the best possible care for their patients.
We hope this article has provided valuable insights into the Healthfirst Medication Prior Authorization Form. If you have any questions or comments, please feel free to share them below.
What is prior authorization, and why is it necessary?
+Prior authorization is a process used by health insurance companies to determine whether a particular medication or treatment is medically necessary and covered under the patient's insurance plan. It helps prevent unnecessary prescriptions, reduces healthcare costs, and promotes the use of evidence-based treatments.
How long does the prior authorization review process take?
+Healthfirst typically reviews prior authorization requests within 24-48 hours. However, the review process may take longer if additional information is required or if the request is submitted during peak periods.
What happens if a prior authorization request is denied?
+If a prior authorization request is denied, healthcare providers can appeal the decision by submitting additional information or supporting documentation. The appeal process typically involves reviewing the denial letter, gathering additional information or supporting documentation, and submitting the appeal request to Healthfirst.