In today's complex healthcare landscape, navigating the intricacies of insurance coverage can be daunting for both healthcare providers and patients. Prior authorization, a critical component of many health insurance plans, is designed to ensure that patients receive medically necessary care while controlling costs. For those enrolled in the Health Plan of San Mateo (HPSM), understanding the prior authorization process is crucial for seamless access to healthcare services. This guide is designed to walk you through the Health Plan of San Mateo's prior authorization process, highlighting its importance, how it works, and what you need to know.

Understanding Prior Authorization
Prior authorization is a process used by health insurance plans to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan. This process is essential for several reasons:
- Ensures Medical Necessity: Prior authorization confirms that the prescribed treatment aligns with evidence-based medical practices and is necessary for the patient's condition.
- Controls Costs: By reviewing treatments before they are administered, insurance plans can manage costs more effectively and reduce unnecessary expenses.
- Improves Safety: The process helps in avoiding treatments that might not be safe or effective for the patient.
How Does Prior Authorization Work?
The prior authorization process typically involves several steps:
- Prescription or Referral: The patient's healthcare provider prescribes a treatment or refers them to a specialist.
- Authorization Request: The healthcare provider or the patient submits a request for prior authorization to the insurance plan, providing detailed information about the treatment and why it is necessary.
- Review: The insurance plan reviews the request, considering factors like medical necessity, alternative treatments, and whether the treatment is covered under the patient's plan.
- Decision: The insurance plan makes a decision to approve, deny, or request more information. This decision is usually communicated to the healthcare provider and the patient.
- Appeal (If Necessary): If the request is denied, the patient or their healthcare provider may appeal the decision, providing additional information to support the request.

The Health Plan of San Mateo (HPSM) Prior Authorization Process
The Health Plan of San Mateo, like other insurance plans, requires prior authorization for certain medical services and treatments. The process is designed to be efficient and patient-centered:
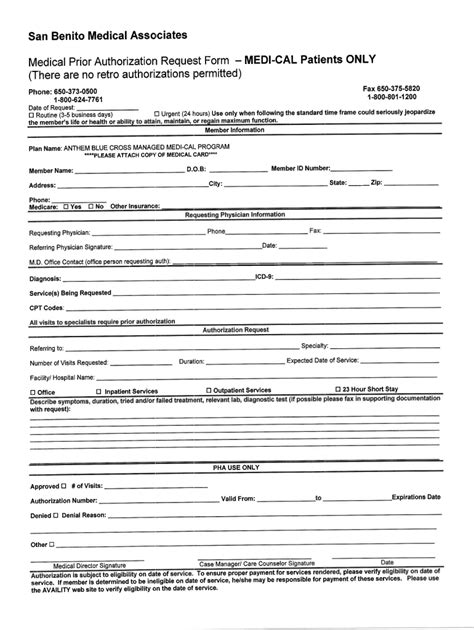
Submitting a Prior Authorization Request
Healthcare providers or patients can submit prior authorization requests through various channels, including online portals, fax, or phone. It's essential to ensure that all required information is included to avoid delays in the review process.
What Requires Prior Authorization?
The Health Plan of San Mateo requires prior authorization for a range of services, including but not limited to:
- Certain medications and drugs
- Surgical procedures
- Specialist consultations
- Durable medical equipment
- Outpatient therapies
A comprehensive list can be found on the HPSM website or by contacting their customer service.

Tips for a Smooth Prior Authorization Process
- Plan Ahead: Allow sufficient time for the prior authorization process to avoid delays in treatment.
- Provide Detailed Information: Ensure that all required information is submitted with the request to facilitate a swift review.
- Stay Informed: Keep track of the status of your prior authorization request and follow up if necessary.
Benefits of Prior Authorization
While the prior authorization process may seem complex, it offers several benefits:
- Cost Savings: By ensuring that only medically necessary treatments are approved, patients can avoid unnecessary medical expenses.
- Improved Patient Safety: The process helps in avoiding treatments that may not be safe or effective.
- Enhanced Patient Outcomes: Prior authorization ensures that patients receive evidence-based treatments, leading to better health outcomes.

Conclusion and Next Steps
Navigating the prior authorization process can seem daunting, but understanding how it works and what is required can make a significant difference. The Health Plan of San Mateo is committed to making this process as efficient and patient-friendly as possible. Whether you're a healthcare provider seeking to understand the process better or a patient looking to ensure access to necessary treatments, staying informed is key.
For more information or to start the prior authorization process, visit the Health Plan of San Mateo's official website or contact their dedicated customer service team. By working together, we can ensure that patients receive the care they need while managing healthcare costs effectively.

We invite you to share your experiences or ask questions about the prior authorization process in the comments section below. Your insights can help others better understand this critical aspect of healthcare management.
What is prior authorization, and why is it necessary?
+Prior authorization is a process used by health insurance plans to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan. It's necessary to ensure that patients receive evidence-based care, control costs, and improve safety.
How do I submit a prior authorization request to the Health Plan of San Mateo?
+You can submit prior authorization requests through the HPSM online portal, by fax, or over the phone. Ensure you have all required information to facilitate a swift review.
What services typically require prior authorization from the Health Plan of San Mateo?
+Services that typically require prior authorization include certain medications, surgical procedures, specialist consultations, durable medical equipment, and outpatient therapies. A comprehensive list is available on the HPSM website.