The Geisinger Health Plan prior authorization form is a crucial document that healthcare providers must complete to ensure that their patients receive the necessary medical treatments and services. However, navigating the prior authorization process can be complex and time-consuming. In this article, we will provide you with 5 tips to help you efficiently complete the Geisinger Health Plan prior auth form and avoid common pitfalls.
Understanding the Prior Authorization Process

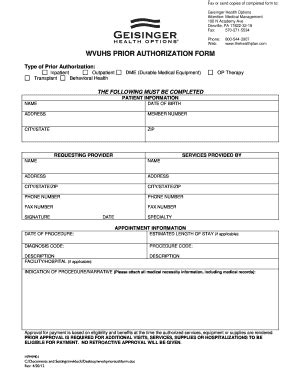
Prior authorization is a process used by health insurance companies to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan. The process typically involves submitting a request to the insurance company, which then reviews the request and makes a determination. In the case of Geisinger Health Plan, the prior authorization form is used to gather information about the patient's condition, the proposed treatment, and the medical necessity of the service.
The Importance of Accurate Information
When completing the Geisinger Health Plan prior auth form, it is essential to provide accurate and detailed information. This includes the patient's demographics, medical history, and current condition, as well as the proposed treatment or service. Inaccurate or incomplete information can lead to delays or denials of the prior authorization request.
Tips for Completing the Geisinger Health Plan Prior Auth Form

Here are 5 tips to help you efficiently complete the Geisinger Health Plan prior auth form:
1. Review the Form Carefully
Before starting to complete the form, review it carefully to ensure that you understand what information is required. The form may include specific instructions or guidelines that must be followed.
2. Gather All Necessary Information
Make sure you have all the necessary information about the patient and the proposed treatment or service. This includes the patient's medical history, current condition, and any relevant test results or documentation.
3. Complete the Form Accurately and Thoroughly
Complete the form accurately and thoroughly, ensuring that all required information is provided. Inaccurate or incomplete information can lead to delays or denials of the prior authorization request.
4. Attach All Required Documentation
Attach all required documentation, including test results, medical records, and any other relevant information. This will help support the prior authorization request and ensure that the insurance company has all the necessary information to make a determination.
5. Submit the Form Promptly
Submit the form promptly to avoid delays in the prior authorization process. The insurance company may have specific deadlines for submitting prior authorization requests, so it is essential to submit the form well in advance of the deadline.
Common Mistakes to Avoid

When completing the Geisinger Health Plan prior auth form, there are several common mistakes to avoid:
- Inaccurate or incomplete information
- Failure to attach required documentation
- Not submitting the form promptly
- Not following specific instructions or guidelines
- Not keeping a copy of the completed form and supporting documentation
The Benefits of Efficient Prior Authorization
Efficient prior authorization can have numerous benefits, including:
- Reduced delays in treatment
- Improved patient outcomes
- Increased patient satisfaction
- Reduced administrative burdens
- Improved communication between healthcare providers and insurance companies
Conclusion
Completing the Geisinger Health Plan prior auth form can be a complex and time-consuming process. However, by following the tips outlined in this article, you can efficiently complete the form and avoid common pitfalls. Remember to review the form carefully, gather all necessary information, complete the form accurately and thoroughly, attach all required documentation, and submit the form promptly.
What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan.
Why is accurate information important on the prior auth form?
+Accurate information is essential to ensure that the insurance company has all the necessary information to make a determination. Inaccurate or incomplete information can lead to delays or denials of the prior authorization request.
What are the benefits of efficient prior authorization?
+Efficient prior authorization can have numerous benefits, including reduced delays in treatment, improved patient outcomes, increased patient satisfaction, reduced administrative burdens, and improved communication between healthcare providers and insurance companies.