Understanding the Importance of Florida Medicaid Prior Authorization Form

For healthcare providers in Florida, navigating the Medicaid prior authorization process can be a complex and time-consuming task. The Florida Medicaid prior authorization form is a crucial document that must be completed accurately and submitted timely to ensure that patients receive the necessary medical treatments and services. In this article, we will provide 5 valuable tips for completing the Florida Medicaid prior authorization form to help healthcare providers streamline their workflow and improve patient care.
The Consequences of Inaccurate or Delayed Submissions
Before we dive into the tips, it's essential to understand the consequences of inaccurate or delayed submissions of the Florida Medicaid prior authorization form. Failure to comply with the prior authorization requirements can result in denied claims, delayed payments, and reduced reimbursement rates. Moreover, inaccurate submissions can lead to audits, fines, and even loss of Medicaid participation. Therefore, it's crucial to ensure that the prior authorization form is completed correctly and submitted on time.
Tips for Completing the Florida Medicaid Prior Authorization Form

Here are 5 valuable tips for completing the Florida Medicaid prior authorization form:
1. Verify Patient Eligibility and Coverage
Before submitting the prior authorization form, verify the patient's eligibility and coverage through the Florida Medicaid website or by contacting the Medicaid helpline. Ensure that the patient's Medicaid ID number is accurate and up-to-date. This step will help prevent denied claims and reduce the risk of delayed payments.
2. Gather Required Documentation
Gather all required documentation, including medical records, test results, and treatment plans, to support the prior authorization request. Ensure that all documentation is accurate, complete, and up-to-date. This will help facilitate the review process and reduce the risk of denied claims.
3. Complete the Form Accurately and Thoroughly
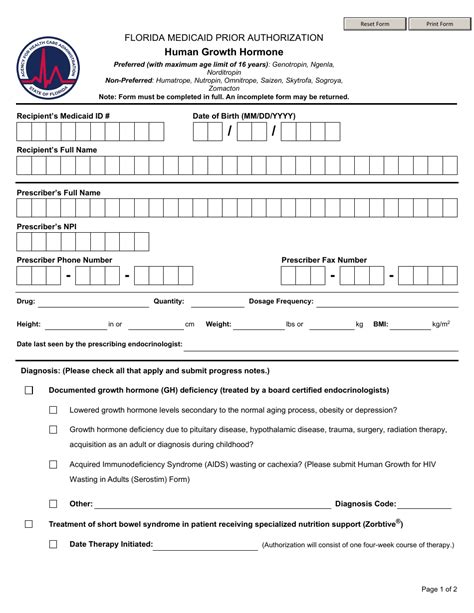
Complete the Florida Medicaid prior authorization form accurately and thoroughly, ensuring that all required fields are filled out correctly. Pay particular attention to the patient's demographic information, diagnosis codes, and treatment plans. Inaccurate or incomplete information can lead to denied claims or delayed payments.
4. Submit the Form Timely
Submit the Florida Medicaid prior authorization form in a timely manner, allowing sufficient time for review and processing. The standard processing time for prior authorization requests is 14 days, but this timeframe may vary depending on the type of service or treatment requested. Ensure that the form is submitted well in advance of the scheduled treatment or service date.
5. Follow Up on the Status of the Request
Follow up on the status of the prior authorization request, contacting the Medicaid helpline or checking the Medicaid website for updates. This will help ensure that the request is processed in a timely manner and that any issues or concerns are addressed promptly.
Best Practices for Streamlining the Prior Authorization Process

In addition to the tips outlined above, here are some best practices for streamlining the prior authorization process:
- Develop a prior authorization workflow that includes clear responsibilities and timelines for each step of the process.
- Designate a prior authorization coordinator or team to manage the process and ensure that requests are submitted accurately and timely.
- Utilize electronic prior authorization tools and software to streamline the submission process and reduce errors.
- Establish relationships with Medicaid representatives and healthcare stakeholders to facilitate communication and resolve issues promptly.
Conclusion
Completing the Florida Medicaid prior authorization form accurately and submitting it timely is crucial for healthcare providers to ensure that patients receive the necessary medical treatments and services. By following the tips outlined above and implementing best practices for streamlining the prior authorization process, healthcare providers can reduce the risk of denied claims, delayed payments, and reduced reimbursement rates. We encourage healthcare providers to take the time to review and understand the prior authorization requirements and to seek guidance from Medicaid representatives or healthcare stakeholders as needed.
What is the purpose of the Florida Medicaid prior authorization form?
+The purpose of the Florida Medicaid prior authorization form is to request approval for medical treatments and services that require prior authorization before they can be covered by Medicaid.
What are the consequences of inaccurate or delayed submissions of the prior authorization form?
+Inaccurate or delayed submissions of the prior authorization form can result in denied claims, delayed payments, and reduced reimbursement rates. Additionally, inaccurate submissions can lead to audits, fines, and even loss of Medicaid participation.
How can healthcare providers streamline the prior authorization process?
+Healthcare providers can streamline the prior authorization process by developing a prior authorization workflow, designating a prior authorization coordinator or team, utilizing electronic prior authorization tools and software, and establishing relationships with Medicaid representatives and healthcare stakeholders.