Prior authorization is a crucial step in ensuring that patients receive the necessary medical treatment while also controlling healthcare costs. Fidelis Care, a New York-based health insurance provider, requires prior authorization for certain medical procedures and medications to ensure that they are medically necessary and cost-effective. In this article, we will provide a comprehensive guide to the Fidelis Care prior authorization form, including the requirements, process, and tips for healthcare providers and patients.
Understanding Prior Authorization
Prior authorization is a process by which healthcare providers obtain approval from a health insurance provider before performing a medical procedure or prescribing a medication. This process is designed to ensure that the treatment is medically necessary, cost-effective, and meets the insurance provider's coverage criteria. Prior authorization helps to prevent unnecessary medical expenses, reduces the risk of adverse reactions, and ensures that patients receive high-quality care.
Fidelis Care Prior Authorization Requirements
Fidelis Care requires prior authorization for certain medical procedures and medications, including:
- Specialist referrals
- Surgical procedures
- High-cost medications
- Experimental treatments
- Durable medical equipment (DME)
Healthcare providers must submit a prior authorization request to Fidelis Care before performing any of these services. The request must include the patient's medical history, diagnosis, treatment plan, and other relevant information.
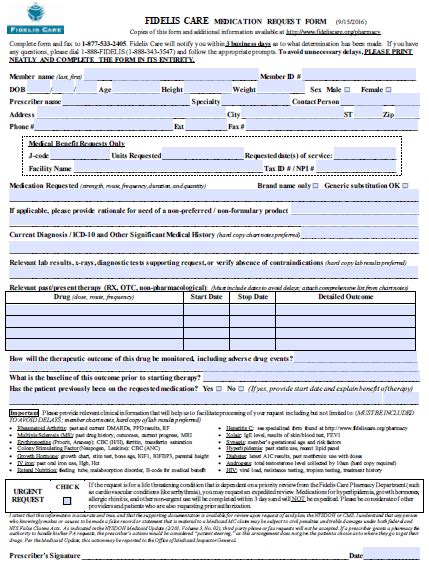
Fidelis Care Prior Authorization Form
The Fidelis Care prior authorization form is used by healthcare providers to submit prior authorization requests to Fidelis Care. The form requires the following information:
- Patient demographics (name, date of birth, policy number)
- Medical history and diagnosis
- Treatment plan and procedure code
- Supporting documentation (medical records, test results, etc.)
- Healthcare provider information (name, address, phone number)

Fidelis Care Prior Authorization Process
The prior authorization process for Fidelis Care involves the following steps:
- Initial Request: The healthcare provider submits a prior authorization request to Fidelis Care via phone, fax, or online portal.
- Review: Fidelis Care reviews the request to determine whether the treatment is medically necessary and meets the insurance provider's coverage criteria.
- Approval or Denial: Fidelis Care issues a decision to approve or deny the prior authorization request.
- Appeal: If the request is denied, the healthcare provider can appeal the decision by submitting additional information or documentation.
Tips for Healthcare Providers
To ensure a smooth prior authorization process, healthcare providers should:
- Verify patient eligibility: Confirm that the patient is eligible for coverage under Fidelis Care.
- Submit complete information: Ensure that all required information is submitted with the prior authorization request.
- Use the correct form: Use the Fidelis Care prior authorization form to submit requests.
- Follow up: Follow up with Fidelis Care to ensure that the request is processed in a timely manner.
Tips for Patients
To ensure that patients receive the necessary medical treatment, patients should:
- Check coverage: Verify that the treatment is covered under Fidelis Care.
- Ask questions: Ask healthcare providers about the prior authorization process and what to expect.
- Provide information: Provide healthcare providers with any necessary information or documentation to support the prior authorization request.
Fidelis Care Prior Authorization FAQs
Q: What is the turnaround time for prior authorization requests? A: Fidelis Care typically processes prior authorization requests within 3-5 business days.
Q: Can I appeal a denied prior authorization request? A: Yes, healthcare providers can appeal a denied prior authorization request by submitting additional information or documentation.
Q: Do I need to submit a prior authorization request for every medical procedure? A: No, prior authorization is only required for certain medical procedures and medications, as determined by Fidelis Care.
What is the Fidelis Care prior authorization form used for?
+The Fidelis Care prior authorization form is used by healthcare providers to submit prior authorization requests to Fidelis Care.
How do I submit a prior authorization request to Fidelis Care?
+Prior authorization requests can be submitted to Fidelis Care via phone, fax, or online portal.
What happens if my prior authorization request is denied?
+If a prior authorization request is denied, healthcare providers can appeal the decision by submitting additional information or documentation.
In conclusion, the Fidelis Care prior authorization form is an essential tool for healthcare providers to ensure that patients receive the necessary medical treatment while also controlling healthcare costs. By following the guidelines and tips outlined in this article, healthcare providers can ensure a smooth prior authorization process and provide high-quality care to their patients.