Receiving medical treatment can be a stressful and overwhelming experience, especially when dealing with insurance providers. One crucial aspect of this process is prior authorization, which can determine whether a specific treatment or medication is covered by your insurance plan. For FEP Blue members, navigating the prior authorization process can be particularly daunting. However, with the right guidance, you can ensure a smoother and more efficient experience.
FEP Blue Prior Authorization Form: Understanding the Basics

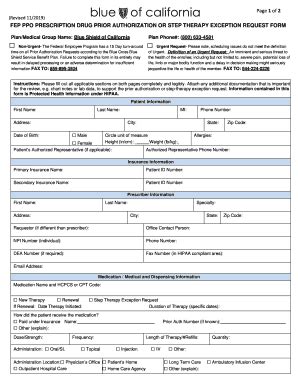
The FEP Blue prior authorization form is a crucial document that requires patients to provide detailed information about their medical condition, treatment plans, and insurance coverage. This form helps FEP Blue determine whether a specific treatment or medication is medically necessary and covered under their plan.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It ensures that patients receive medically necessary treatments and medications.
- It helps prevent unnecessary or duplicate treatments.
- It reduces healthcare costs by avoiding unnecessary procedures.
- It enables insurance providers to manage their costs and ensure that patients receive high-quality care.
Step 1: Gather Required Information and Documents

Before starting the prior authorization process, it's essential to gather all required information and documents. This includes:
- Your FEP Blue insurance card
- Your medical records and test results
- A detailed description of your medical condition and treatment plan
- A list of your medications and dosages
- Your doctor's contact information and signature
Step 1.1: Verify Your Insurance Coverage
Before submitting the prior authorization form, verify your insurance coverage to ensure that the treatment or medication is covered under your plan. You can do this by:
- Checking your insurance policy documents
- Contacting FEP Blue customer service
- Visiting the FEP Blue website
Step 2: Fill Out the Prior Authorization Form

Once you have gathered all required information and documents, it's time to fill out the prior authorization form. Make sure to:
- Fill out the form accurately and completely
- Include all required information and documents
- Sign and date the form
Step 2.1: Submit the Form
After completing the form, submit it to FEP Blue for review. You can do this by:
- Faxing the form to FEP Blue
- Mailing the form to FEP Blue
- Submitting the form online through the FEP Blue website
Step 3: Wait for FEP Blue's Review and Decision

After submitting the prior authorization form, wait for FEP Blue's review and decision. This may take several days or weeks, depending on the complexity of the case.
Step 3.1: Follow Up with FEP Blue
If you haven't received a decision within the expected timeframe, follow up with FEP Blue to inquire about the status of your request. You can do this by:
- Contacting FEP Blue customer service
- Checking the status of your request online through the FEP Blue website
Step 4: Receive FEP Blue's Decision

Once FEP Blue has reviewed your request, they will send you a decision letter outlining their determination. If your request is approved, you can proceed with the treatment or medication. If your request is denied, you may appeal the decision.
Step 4.1: Appeal FEP Blue's Decision (If Necessary)
If FEP Blue denies your request, you may appeal the decision. To do this, you'll need to:
- Review FEP Blue's decision letter to understand the reason for the denial
- Gather additional information and documentation to support your appeal
- Submit a written appeal to FEP Blue within the specified timeframe
Step 5: Follow Up with Your Healthcare Provider

After receiving FEP Blue's decision, follow up with your healthcare provider to:
- Discuss the outcome of the prior authorization request
- Schedule the treatment or medication (if approved)
- Explore alternative treatment options (if denied)
Conclusion
Navigating the FEP Blue prior authorization process can be complex and time-consuming. However, by following these 5 easy steps, you can ensure a smoother and more efficient experience. Remember to gather all required information and documents, fill out the form accurately and completely, and follow up with FEP Blue and your healthcare provider as needed.
What is prior authorization, and why is it necessary?
+Prior authorization is a process that determines whether a specific treatment or medication is medically necessary and covered under your insurance plan. It's necessary to ensure that patients receive high-quality care while managing healthcare costs.
How long does the prior authorization process take?
+The prior authorization process can take several days or weeks, depending on the complexity of the case. It's essential to follow up with FEP Blue and your healthcare provider to ensure a smooth and efficient experience.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you may appeal the decision. To do this, you'll need to review FEP Blue's decision letter, gather additional information and documentation, and submit a written appeal to FEP Blue within the specified timeframe.