Navigating the complexities of healthcare can be a daunting task, especially for federal employees. One crucial aspect of this process is the prior authorization form, a necessary step in ensuring that patients receive the care they need. In this article, we will delve into the world of Federal Employee Program (FEP) prior authorization form requirements, exploring the importance of this process, its benefits, and the steps involved.

What is Prior Authorization, and Why is it Necessary?
Prior authorization is a process used by health insurance companies to determine whether a specific treatment or medication is medically necessary. This step is essential in ensuring that patients receive the most effective and cost-efficient care possible. By reviewing the medical necessity of a particular treatment, prior authorization helps prevent unnecessary procedures and reduces healthcare costs.
Benefits of Prior Authorization
The prior authorization process offers several benefits to patients, healthcare providers, and insurance companies alike. Some of the key advantages include:
- Ensures medically necessary treatments: Prior authorization helps ensure that patients receive treatments that are medically necessary, reducing the risk of unnecessary procedures.
- Reduces healthcare costs: By preventing unnecessary treatments, prior authorization helps reduce healthcare costs, which can lead to lower premiums and out-of-pocket expenses for patients.
- Promotes communication: The prior authorization process encourages communication between healthcare providers, patients, and insurance companies, ensuring that all parties are informed and involved in the decision-making process.
FEP Prior Authorization Form Requirements
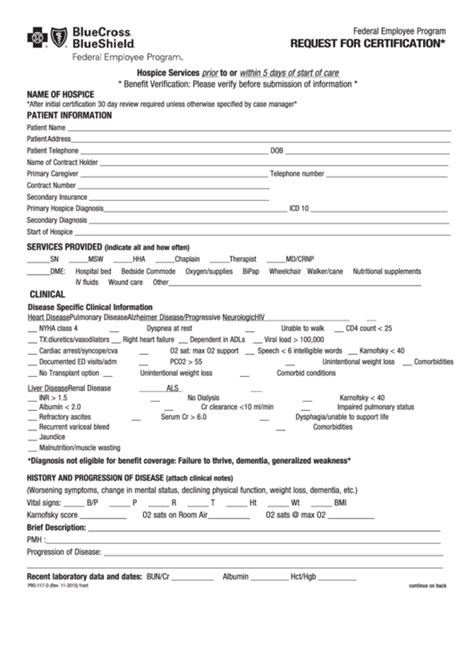
The Federal Employee Program (FEP) prior authorization form requirements are specific to the FEP Blue Cross Blue Shield (BCBS) insurance plan. To ensure a smooth prior authorization process, it is essential to understand the requirements and steps involved.

Required Information
When submitting a prior authorization request, the following information is typically required:
- Patient demographics: Name, date of birth, and contact information
- Healthcare provider information: Name, address, and contact information
- Treatment or medication details: Type, dosage, and duration of treatment
- Medical necessity documentation: Supporting documentation, such as medical records and test results, to justify the treatment or medication
Steps Involved in the Prior Authorization Process
The prior authorization process typically involves the following steps:
Step 1: Submitting the Request
The healthcare provider or patient submits a prior authorization request to the FEP BCBS insurance company. This can be done electronically or by mail.

Step 2: Review and Verification
The FEP BCBS insurance company reviews and verifies the information submitted, ensuring that all necessary documentation is included.
Step 3: Determination and Notification
The FEP BCBS insurance company makes a determination regarding the prior authorization request and notifies the healthcare provider and patient of the decision.
Common Challenges and Solutions
Despite the importance of prior authorization, the process can be complex and time-consuming. Some common challenges and solutions include:
Challenge 1: Incomplete or Missing Information
Solution: Ensure that all necessary information is submitted with the prior authorization request, and verify that all documentation is complete and accurate.
Challenge 2: Delayed or Denied Requests
Solution: Submit prior authorization requests in a timely manner, and follow up with the FEP BCBS insurance company to ensure that the request is being processed.

Best Practices for a Smooth Prior Authorization Process
To ensure a smooth prior authorization process, follow these best practices:
- Submit complete and accurate information
- Verify that all necessary documentation is included
- Submit requests in a timely manner
- Follow up with the FEP BCBS insurance company to ensure that the request is being processed
Conclusion
The Federal Employee Program prior authorization form requirements are an essential aspect of the healthcare process. By understanding the requirements and steps involved, patients and healthcare providers can ensure a smooth and efficient prior authorization process. Remember to submit complete and accurate information, verify that all necessary documentation is included, and follow up with the FEP BCBS insurance company to ensure that the request is being processed.

We hope that this article has provided valuable insights into the world of FEP prior authorization form requirements. If you have any questions or comments, please feel free to share them below.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a specific treatment or medication is medically necessary.
What information is required for a prior authorization request?
+Patient demographics, healthcare provider information, treatment or medication details, and medical necessity documentation are typically required.
How long does the prior authorization process take?
+The prior authorization process typically takes several days to several weeks, depending on the complexity of the request and the insurance company's processing time.