As a federal employee, navigating the complexities of health insurance can be overwhelming. One crucial aspect of managing your healthcare benefits is understanding the FEP prior authorization form. In this article, we will delve into the world of FEP prior authorization, explaining its purpose, benefits, and the step-by-step process of completing the form.

What is FEP Prior Authorization?
FEP prior authorization is a process required by the Federal Employees Health Benefits (FEHB) program to ensure that certain medical treatments, procedures, and prescriptions are necessary and cost-effective. The FEHB program is designed to provide comprehensive health insurance coverage to federal employees, retirees, and their families. Prior authorization helps to prevent unnecessary medical expenses and ensures that patients receive the most appropriate care.
Benefits of FEP Prior Authorization
The FEP prior authorization process offers several benefits, including:
- Reduced healthcare costs: By reviewing medical treatments and prescriptions, prior authorization helps to prevent unnecessary expenses and ensures that patients receive the most cost-effective care.
- Improved patient outcomes: Prior authorization ensures that patients receive the most appropriate treatment, reducing the risk of adverse reactions and improving overall health outcomes.
- Enhanced patient safety: By reviewing medical treatments and prescriptions, prior authorization helps to identify potential safety risks and prevent adverse reactions.
The FEP Prior Authorization Form: A Step-by-Step Guide
Completing the FEP prior authorization form can seem daunting, but by following these steps, you can ensure a smooth and efficient process.

Step 1: Gather Required Information
Before starting the prior authorization process, you will need to gather the required information, including:
- Your FEHB plan identification number
- Your patient's name and date of birth
- The treatment, procedure, or prescription being requested
- The date and duration of the treatment, procedure, or prescription
- The medical reason for the treatment, procedure, or prescription
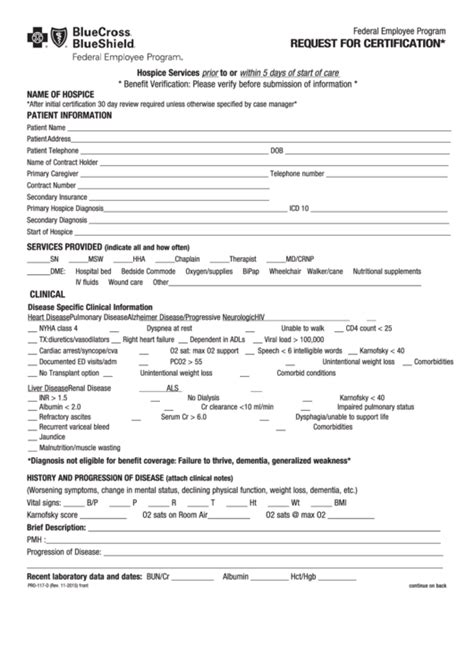
Step 2: Complete the FEP Prior Authorization Form
Once you have gathered the required information, you can complete the FEP prior authorization form. The form will require you to provide the following information:
- Patient information
- Treatment, procedure, or prescription information
- Medical reason for the treatment, procedure, or prescription
- Supporting documentation, such as medical records or test results
Step 3: Submit the FEP Prior Authorization Form
After completing the FEP prior authorization form, you will need to submit it to your FEHB plan for review. You can submit the form online, by phone, or by mail, depending on your plan's requirements.
Common FEP Prior Authorization Requirements
While the FEP prior authorization form may vary depending on your FEHB plan, there are some common requirements that you should be aware of.

Medical Necessity
One of the primary requirements for FEP prior authorization is medical necessity. Your FEHB plan will review your request to ensure that the treatment, procedure, or prescription is medically necessary and aligns with established medical guidelines.
Cost-Effectiveness
Another key requirement is cost-effectiveness. Your FEHB plan will review your request to ensure that the treatment, procedure, or prescription is the most cost-effective option available.
Tips for a Smooth FEP Prior Authorization Process
To ensure a smooth FEP prior authorization process, follow these tips:
- Review your FEHB plan's prior authorization requirements carefully
- Gather all required information before submitting your request
- Submit your request well in advance of the treatment, procedure, or prescription date
- Follow up with your FEHB plan to ensure that your request is being processed

Conclusion
In conclusion, the FEP prior authorization form is an essential part of managing your healthcare benefits as a federal employee. By understanding the purpose, benefits, and step-by-step process of completing the form, you can ensure a smooth and efficient prior authorization process. Remember to review your FEHB plan's requirements carefully, gather all required information, and submit your request well in advance of the treatment, procedure, or prescription date.

We encourage you to share your experiences with the FEP prior authorization process in the comments below. Your insights can help other federal employees navigate the complexities of healthcare benefits.
What is the purpose of FEP prior authorization?
+The purpose of FEP prior authorization is to ensure that certain medical treatments, procedures, and prescriptions are necessary and cost-effective.
How do I submit a FEP prior authorization request?
+You can submit a FEP prior authorization request online, by phone, or by mail, depending on your FEHB plan's requirements.
What information do I need to provide for FEP prior authorization?
+You will need to provide your FEHB plan identification number, patient information, treatment, procedure, or prescription information, and supporting documentation, such as medical records or test results.