The complexities of healthcare insurance can be overwhelming, especially when it comes to prior authorization. Federal BCBS (Blue Cross Blue Shield) prior authorization is a process that can seem daunting, but it doesn't have to be. In this article, we'll break down the process into 5 easy steps, making it easier for you to navigate and ensure that you receive the medical care you need.
What is Federal BCBS Prior Authorization?

Prior authorization is a process used by health insurance companies to determine whether a specific treatment or medication is medically necessary. For Federal BCBS, prior authorization is required for certain services, including prescription medications, medical procedures, and durable medical equipment. The goal of prior authorization is to ensure that patients receive safe and effective treatment while also controlling healthcare costs.
Step 1: Verify Prior Authorization Requirements

The first step in the prior authorization process is to verify whether prior authorization is required for your specific treatment or medication. You can do this by:
- Checking your Federal BCBS insurance policy documents
- Contacting your healthcare provider or their office staff
- Visiting the Federal BCBS website or contacting their customer service
Important Documents Needed
To verify prior authorization requirements, you'll need to have the following documents ready:
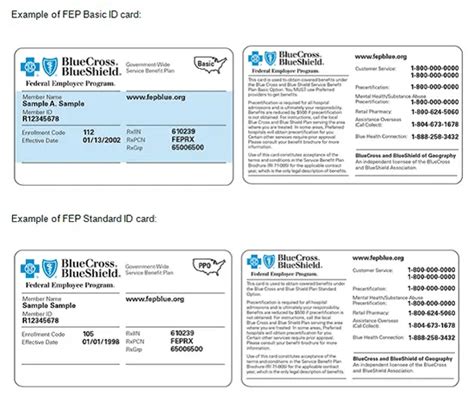
- Your Federal BCBS insurance card
- A list of your medications and medical conditions
- A copy of your prescription or treatment plan
Step 2: Gather Required Information and Documents

Once you've verified that prior authorization is required, you'll need to gather the necessary information and documents to submit with your request. This may include:
- Your medical history and diagnosis
- Treatment options and recommendations from your healthcare provider
- Supporting documentation, such as test results or medical records
- A completed prior authorization form, which can be obtained from Federal BCBS or your healthcare provider
Tips for Gathering Information
- Be sure to ask your healthcare provider or their office staff for help gathering the necessary information and documents.
- Keep a copy of all documents and information submitted for your records.
- Double-check that all information is accurate and complete to avoid delays in the prior authorization process.
Step 3: Submit Your Prior Authorization Request

With all the necessary information and documents in hand, you can submit your prior authorization request to Federal BCBS. You can do this by:
- Faxing the completed prior authorization form and supporting documentation to Federal BCBS
- Mailing the completed prior authorization form and supporting documentation to Federal BCBS
- Submitting the request online through the Federal BCBS website or patient portal
Submission Tips
- Be sure to follow the submission guidelines carefully to avoid delays.
- Keep a copy of the submitted request and supporting documentation for your records.
- Follow up with Federal BCBS to confirm receipt of your request.
Step 4: Wait for a Decision and Follow Up

After submitting your prior authorization request, you'll need to wait for a decision from Federal BCBS. This can take several days or weeks, depending on the complexity of the request and the speed of the review process.
- Follow up with Federal BCBS to check on the status of your request
- Be prepared to provide additional information or documentation if requested
Understanding the Decision
- If your request is approved, you'll receive notification from Federal BCBS, and you can proceed with the treatment or medication.
- If your request is denied, you'll receive notification from Federal BCBS, and you may be able to appeal the decision.
Step 5: Appeal the Decision (If Necessary)

If your prior authorization request is denied, you may be able to appeal the decision. This involves submitting additional information or documentation to support your request.
- Review the denial notification from Federal BCBS to understand the reasons for the denial
- Gather additional information or documentation to support your appeal
- Submit the appeal to Federal BCBS, following their guidelines and procedures
Avoiding Delays
- Be sure to follow the appeal guidelines carefully to avoid delays.
- Keep a copy of the appeal and supporting documentation for your records.
- Follow up with Federal BCBS to confirm receipt of your appeal.
What is prior authorization, and why is it required?
+Prior authorization is a process used by health insurance companies to determine whether a specific treatment or medication is medically necessary. It's required for certain services, including prescription medications, medical procedures, and durable medical equipment, to ensure that patients receive safe and effective treatment while also controlling healthcare costs.
How long does the prior authorization process take?
+The prior authorization process can take several days or weeks, depending on the complexity of the request and the speed of the review process.
What if my prior authorization request is denied?
+If your prior authorization request is denied, you may be able to appeal the decision. This involves submitting additional information or documentation to support your request.
By following these 5 easy steps, you can navigate the Federal BCBS prior authorization process with confidence. Remember to stay organized, follow the guidelines carefully, and don't hesitate to ask for help if you need it. If you have any further questions or concerns, please don't hesitate to comment below or share this article with others who may find it helpful.