Streamlining healthcare processes is crucial for efficient patient care and reduced administrative burdens. One essential aspect of healthcare management is prior authorization, which ensures that patients receive necessary treatments while minimizing unnecessary costs. The Envolve prior authorization form plays a vital role in this process, allowing healthcare providers to quickly and easily obtain approval for treatments. In this article, we will delve into the world of prior authorization, explore the benefits of using the Envolve prior authorization form, and discuss how it can help streamline your healthcare operations.
Understanding Prior Authorization
Prior authorization is a process used by healthcare payers to determine whether a particular treatment or medication is medically necessary and covered under a patient's insurance plan. This process typically involves a healthcare provider submitting a request for approval before administering the treatment or prescribing the medication. The goal of prior authorization is to ensure that patients receive only necessary and effective treatments, reducing unnecessary costs and improving health outcomes.

Benefits of Prior Authorization
Prior authorization offers numerous benefits for both patients and healthcare providers. Some of the most significant advantages include:
- Improved patient outcomes: By ensuring that patients receive only medically necessary treatments, prior authorization can help improve health outcomes and reduce the risk of adverse reactions.
- Reduced costs: Prior authorization can help reduce healthcare costs by minimizing unnecessary treatments and medications.
- Enhanced patient safety: Prior authorization can help identify potential safety concerns, such as drug interactions or allergic reactions, before treatments are administered.
- Streamlined administrative processes: Prior authorization can help reduce administrative burdens by automating the approval process and minimizing paperwork.
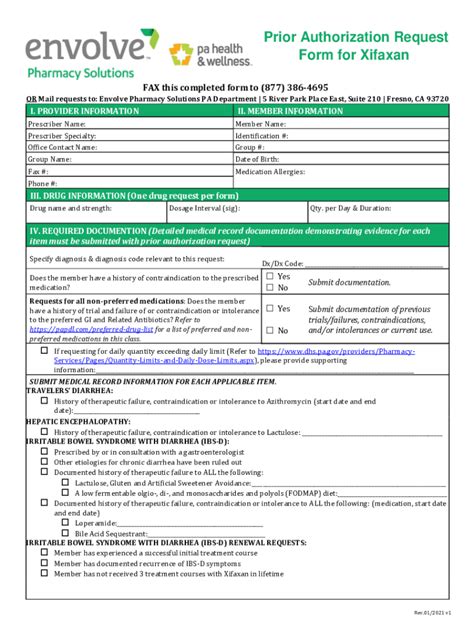
The Envolve Prior Authorization Form
The Envolve prior authorization form is a comprehensive tool designed to simplify the prior authorization process. This form allows healthcare providers to quickly and easily submit requests for approval, reducing administrative burdens and minimizing delays. The Envolve prior authorization form typically includes the following information:
- Patient demographics and insurance information
- Treatment or medication details, including dosage and frequency
- Medical necessity documentation, including diagnosis and treatment plans
- Supporting documentation, such as lab results or medical records

Benefits of Using the Envolve Prior Authorization Form
Using the Envolve prior authorization form offers numerous benefits for healthcare providers, including:
- Streamlined administrative processes: The Envolve prior authorization form can help reduce administrative burdens by automating the approval process and minimizing paperwork.
- Improved patient outcomes: By ensuring that patients receive only medically necessary treatments, the Envolve prior authorization form can help improve health outcomes and reduce the risk of adverse reactions.
- Enhanced patient safety: The Envolve prior authorization form can help identify potential safety concerns, such as drug interactions or allergic reactions, before treatments are administered.
- Reduced costs: The Envolve prior authorization form can help reduce healthcare costs by minimizing unnecessary treatments and medications.
How to Use the Envolve Prior Authorization Form
Using the Envolve prior authorization form is a straightforward process that can be completed in a few simple steps:
- Download the Envolve prior authorization form from the Envolve website or access it through your electronic health record (EHR) system.
- Complete the form with the required information, including patient demographics, treatment or medication details, and medical necessity documentation.
- Attach supporting documentation, such as lab results or medical records, as needed.
- Submit the form to Envolve for review and approval.

Common Challenges and Solutions
While the Envolve prior authorization form can help streamline the prior authorization process, there are some common challenges that healthcare providers may encounter. Some of the most common challenges and solutions include:
- Delays in approval: To minimize delays, ensure that all required information is included on the form and that supporting documentation is attached as needed.
- Denials: To minimize denials, ensure that the treatment or medication is medically necessary and that the form is completed accurately and thoroughly.
- Administrative burdens: To minimize administrative burdens, consider using an electronic prior authorization system that can automate the approval process and minimize paperwork.
Best Practices for Using the Envolve Prior Authorization Form
To get the most out of the Envolve prior authorization form, consider the following best practices:
- Ensure that all required information is included on the form and that supporting documentation is attached as needed.
- Use an electronic prior authorization system to automate the approval process and minimize paperwork.
- Ensure that the treatment or medication is medically necessary and that the form is completed accurately and thoroughly.
- Follow up with Envolve to ensure that the request is processed in a timely manner.

Conclusion
The Envolve prior authorization form is a valuable tool that can help streamline the prior authorization process and improve patient outcomes. By understanding the benefits and challenges of prior authorization, healthcare providers can use the Envolve prior authorization form to minimize administrative burdens, reduce costs, and enhance patient safety. By following best practices and using an electronic prior authorization system, healthcare providers can get the most out of the Envolve prior authorization form and provide high-quality patient care.

We hope this article has provided valuable insights into the world of prior authorization and the benefits of using the Envolve prior authorization form. If you have any questions or comments, please don't hesitate to reach out. Share this article with your colleagues and friends to help spread the word about the importance of streamlined prior authorization processes.
What is prior authorization?
+Prior authorization is a process used by healthcare payers to determine whether a particular treatment or medication is medically necessary and covered under a patient's insurance plan.
What is the Envolve prior authorization form?
+The Envolve prior authorization form is a comprehensive tool designed to simplify the prior authorization process. It allows healthcare providers to quickly and easily submit requests for approval, reducing administrative burdens and minimizing delays.
What are the benefits of using the Envolve prior authorization form?
+The Envolve prior authorization form offers numerous benefits, including streamlined administrative processes, improved patient outcomes, enhanced patient safety, and reduced costs.