The healthcare industry is a complex and multifaceted system, with various stakeholders working together to provide quality care to patients. One crucial aspect of this system is the prior authorization process, which ensures that patients receive necessary treatments while also controlling healthcare costs. Empirx Health is a leading provider of prior authorization solutions, and their prior authorization form is an essential tool for healthcare professionals. In this article, we will delve into the world of prior authorization, explore the Empirx Health prior authorization form, and provide a simplified guide to help you navigate this process.
Understanding Prior Authorization

Prior authorization is a process used by healthcare payers to determine whether a specific treatment or medication is medically necessary and covered under a patient's insurance plan. This process involves reviewing the patient's medical history, diagnosis, and treatment plan to ensure that the requested service is appropriate and necessary. Prior authorization is usually required for high-cost or specialty medications, surgical procedures, and other treatments that require careful consideration.
The Importance of Prior Authorization
Prior authorization plays a crucial role in the healthcare system, as it helps to:
- Control healthcare costs by ensuring that only necessary treatments are approved
- Improve patient outcomes by ensuring that patients receive evidence-based treatments
- Reduce administrative burdens on healthcare providers by streamlining the approval process
- Enhance patient safety by reducing the risk of adverse reactions or interactions
The Empirx Health Prior Authorization Form

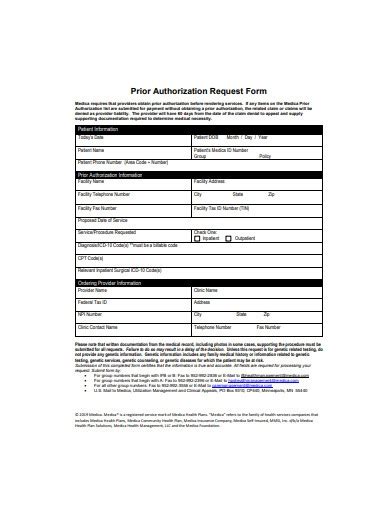
The Empirx Health prior authorization form is a comprehensive document that requires healthcare providers to submit detailed information about the patient's condition, treatment plan, and medical history. The form typically includes sections for:
- Patient demographics and insurance information
- Medical history and diagnosis
- Treatment plan and medication list
- Supporting documentation, such as lab results or medical records
Completing the Empirx Health Prior Authorization Form
To complete the Empirx Health prior authorization form, healthcare providers should:
- Ensure that all required fields are completed accurately and thoroughly
- Provide clear and concise documentation to support the treatment plan
- Submit the form electronically or by mail, depending on the payer's requirements
- Follow up with the payer to ensure that the form is received and processed in a timely manner
Benefits of Using the Empirx Health Prior Authorization Form

The Empirx Health prior authorization form offers several benefits to healthcare providers, including:
- Streamlined approval process: The form is designed to make it easy for providers to submit necessary information, reducing the risk of delays or denials.
- Improved patient outcomes: By ensuring that patients receive necessary treatments, the form helps to improve patient outcomes and quality of care.
- Reduced administrative burdens: The form is designed to minimize administrative tasks, allowing providers to focus on patient care.
Common Challenges with Prior Authorization
Despite the benefits of prior authorization, healthcare providers often face challenges with the process, including:
- Delays in approval: Prior authorization can delay treatment, which can negatively impact patient outcomes.
- Denials: Providers may experience denials due to incomplete or inaccurate information.
- Administrative burdens: The prior authorization process can be time-consuming and administratively burdensome.
Best Practices for Prior Authorization

To overcome common challenges with prior authorization, healthcare providers can follow best practices, including:
- Ensuring accurate and complete information: Providers should carefully review the prior authorization form to ensure that all required fields are completed accurately and thoroughly.
- Submitting supporting documentation: Providers should submit supporting documentation, such as lab results or medical records, to support the treatment plan.
- Following up with payers: Providers should follow up with payers to ensure that the form is received and processed in a timely manner.
Conclusion
In conclusion, the Empirx Health prior authorization form is an essential tool for healthcare providers, as it helps to ensure that patients receive necessary treatments while also controlling healthcare costs. By understanding the prior authorization process and following best practices, providers can overcome common challenges and improve patient outcomes.
Additional Resources

For more information on prior authorization and the Empirx Health prior authorization form, providers can access additional resources, including:
- Empirx Health website: Providers can visit the Empirx Health website to access the prior authorization form and learn more about the prior authorization process.
- Payer websites: Providers can visit payer websites to learn more about specific prior authorization requirements and guidelines.
Engage with Us
We hope this article has provided valuable insights into the Empirx Health prior authorization form and the prior authorization process. If you have any questions or comments, please feel free to share them with us. We would love to hear from you!
What is prior authorization?
+Prior authorization is a process used by healthcare payers to determine whether a specific treatment or medication is medically necessary and covered under a patient's insurance plan.
Why is prior authorization important?
+Prior authorization is important because it helps to control healthcare costs, improve patient outcomes, and reduce administrative burdens on healthcare providers.
How do I complete the Empirx Health prior authorization form?
+To complete the Empirx Health prior authorization form, healthcare providers should ensure that all required fields are completed accurately and thoroughly, provide clear and concise documentation to support the treatment plan, and submit the form electronically or by mail, depending on the payer's requirements.