As the healthcare landscape continues to evolve, patients and healthcare providers alike are often faced with the daunting task of navigating complex administrative processes. One such process that can be particularly confusing is the prior authorization form for Elderplan, a specialized health insurance program designed for low-income seniors and individuals with disabilities. In this article, we will break down the prior authorization process into 5 easy steps, providing clarity and guidance for those seeking to access essential healthcare services.
Understanding the Importance of Prior Authorization

Prior authorization, also known as pre-certification or pre-authorization, is a process used by health insurance companies to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan. This process is designed to ensure that patients receive necessary and effective care while also controlling healthcare costs. For Elderplan members, prior authorization is a crucial step in accessing specialized care, such as hospitalizations, surgeries, and prescription medications.
Step 1: Reviewing the Elderplan Prior Authorization Requirements

Before initiating the prior authorization process, it is essential to review the specific requirements for Elderplan. This includes:
- Verifying the patient's eligibility and coverage under the Elderplan program
- Identifying the type of service or treatment requiring prior authorization
- Gathering relevant medical documentation, such as patient history, diagnosis, and treatment plans
- Understanding the necessary forms and paperwork required for submission
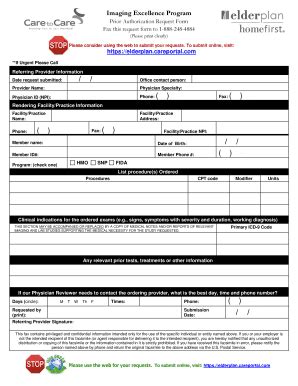
Elderplan Prior Authorization Forms and Documents
To facilitate a smooth prior authorization process, the following forms and documents may be required:
- Elderplan Prior Authorization Request Form
- Patient's medical records and history
- Treatment plans and medication lists
- Diagnostic test results and reports
- Letter of medical necessity from the treating physician
Step 2: Submitting the Prior Authorization Request

Once the necessary forms and documents are gathered, the prior authorization request can be submitted to Elderplan. This can typically be done via:
- Fax: Submitting the request and supporting documents via fax to the designated Elderplan fax number
- Mail: Mailing the request and supporting documents to the designated Elderplan mailing address
- Online Portal: Submitting the request and supporting documents through the Elderplan online portal (if available)
Step 3: Review and Determination

After receiving the prior authorization request, Elderplan will review the submission to determine whether the requested service or treatment is medically necessary and covered under the patient's insurance plan. This review process typically takes several days to several weeks, depending on the complexity of the request and the availability of necessary information.
Elderplan Prior Authorization Determination
The prior authorization determination will be communicated to the patient and the treating physician via:
- Letter or email notification
- Phone call or voicemail
- Online portal notification (if available)
Step 4: Receiving Approval or Denial

Upon completion of the review process, Elderplan will render a decision on the prior authorization request. If approved, the patient will be notified of the approved service or treatment, and the necessary arrangements can be made. If denied, the patient and treating physician will receive a notification explaining the reason for the denial and any potential next steps.
Step 5: Appealing a Denial (If Necessary)

If the prior authorization request is denied, the patient and treating physician may appeal the decision. This involves submitting additional information or documentation to support the requested service or treatment. The appeals process typically follows a standard protocol, which may include:
- Submitting a written appeal within a specified timeframe
- Providing additional medical documentation or supporting evidence
- Participating in a phone or in-person review with an Elderplan representative
We encourage readers to share their experiences with the Elderplan prior authorization process in the comments below. If you have any questions or concerns, please feel free to ask. Additionally, if you found this article informative, please share it with others who may benefit from this information.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan.
What forms and documents are required for Elderplan prior authorization?
+The necessary forms and documents may include the Elderplan Prior Authorization Request Form, patient's medical records and history, treatment plans and medication lists, diagnostic test results and reports, and a letter of medical necessity from the treating physician.
How long does the prior authorization process typically take?
+The prior authorization process typically takes several days to several weeks, depending on the complexity of the request and the availability of necessary information.