Credence BCBS Prior Authorization Form: A Comprehensive Guide

Prior authorization is a crucial step in the healthcare process, ensuring that patients receive necessary treatments while controlling costs. For Credence BCBS (Blue Cross Blue Shield) members, understanding the prior authorization form is essential for accessing medical services. In this article, we will delve into the Credence BCBS prior authorization form, exploring its importance, the process of submission, and providing a step-by-step guide.
What is the Credence BCBS Prior Authorization Form?
The Credence BCBS prior authorization form is a document used by healthcare providers to request approval for specific treatments, medications, or services for patients insured by Credence BCBS. This form is a crucial part of the prior authorization process, which helps ensure that patients receive necessary care while minimizing unnecessary costs.
Why is Prior Authorization Important?

Prior authorization is essential in the healthcare system for several reasons:
- Cost Control: Prior authorization helps control healthcare costs by ensuring that patients receive only necessary treatments.
- Improved Patient Care: By reviewing treatment requests, prior authorization promotes high-quality patient care and reduces the risk of adverse reactions or unnecessary procedures.
- Reduced Administrative Burden: The prior authorization process streamlines the administrative tasks associated with treatment approval, making it more efficient for healthcare providers.
How to Submit a Credence BCBS Prior Authorization Form
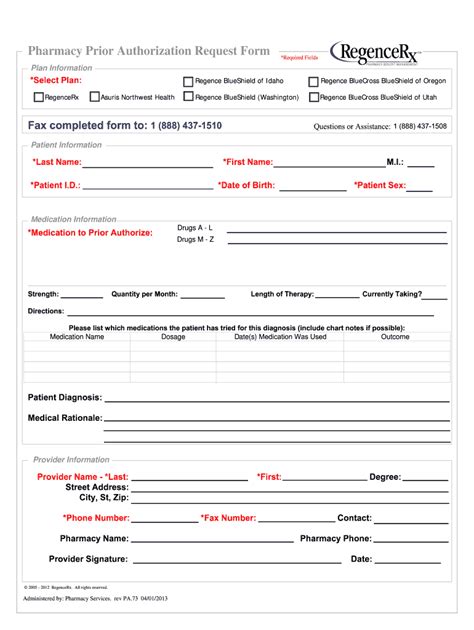
Submitting a Credence BCBS prior authorization form involves several steps:
- Gather Required Information: Healthcare providers must collect patient information, medical records, and treatment details before submitting the form.
- Complete the Form: The prior authorization form must be completed accurately and thoroughly, including all required information and supporting documentation.
- Submit the Form: The completed form can be submitted via fax, mail, or online portal, depending on the Credence BCBS requirements.
Credence BCBS Prior Authorization Form Requirements

To ensure a smooth prior authorization process, healthcare providers must meet the following requirements:
- Accurate Patient Information: Patient demographics, medical history, and current treatment plans must be accurate and up-to-date.
- Complete Medical Records: Relevant medical records, test results, and treatment plans must be included with the prior authorization form.
- Clear Treatment Details: A detailed description of the requested treatment, including dosage, frequency, and duration, must be provided.
Tips for a Successful Prior Authorization Submission
To increase the chances of a successful prior authorization submission, healthcare providers can follow these tips:
- Verify Patient Eligibility: Confirm patient eligibility and coverage before submitting the prior authorization form.
- Use Correct Coding: Ensure that all medical codes, including ICD-10 and CPT codes, are accurate and up-to-date.
- Include Supporting Documentation: Provide all relevant supporting documentation, including medical records and test results.
Credence BCBS Prior Authorization Form FAQ

Frequently Asked Questions about the Credence BCBS prior authorization form:
- Q: What is the purpose of the prior authorization form?
- A: The prior authorization form is used to request approval for specific treatments, medications, or services for patients insured by Credence BCBS.
- Q: How do I submit a prior authorization form?
- A: The completed form can be submitted via fax, mail, or online portal, depending on the Credence BCBS requirements.
- Q: What information is required on the prior authorization form?
- A: The form requires patient information, medical records, and treatment details, including dosage, frequency, and duration.
What is the typical turnaround time for prior authorization requests?
+The typical turnaround time for prior authorization requests is 3-5 business days. However, this may vary depending on the complexity of the request and the availability of required information.
Can I check the status of my prior authorization request online?
+Yes, you can check the status of your prior authorization request online through the Credence BCBS provider portal or by contacting their customer service department.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you will receive a notification explaining the reason for the denial. You can appeal the decision by submitting additional information or requesting a peer-to-peer review.
By understanding the Credence BCBS prior authorization form and following the guidelines outlined in this article, healthcare providers can ensure a smooth and efficient prior authorization process, ultimately improving patient care and reducing administrative burdens.