CountyCare is a Medicaid managed care program that provides healthcare services to eligible individuals in Cook County, Illinois. As a healthcare provider, navigating the prior authorization process can be challenging, but understanding the steps involved can help streamline the process. In this article, we will guide you through the 5 easy steps for CountyCare prior authorization form.

Understanding CountyCare Prior Authorization
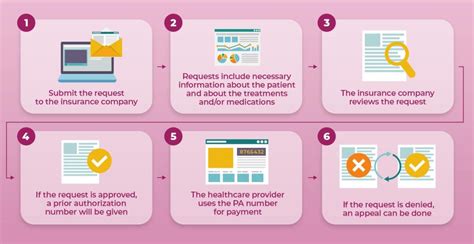
Prior authorization is a process that requires healthcare providers to obtain approval from CountyCare before providing certain medical services or prescribing specific medications to patients. This process helps ensure that patients receive medically necessary care while minimizing unnecessary costs.
Benefits of Prior Authorization
The prior authorization process offers several benefits, including:
- Ensures that patients receive medically necessary care
- Reduces unnecessary healthcare costs
- Promotes communication between healthcare providers and CountyCare
- Enhances patient safety by preventing unnecessary or contraindicated treatments
Step 1: Determine If Prior Authorization Is Required

Before initiating the prior authorization process, it's essential to determine if prior authorization is required for the specific service or medication. You can check the CountyCare website or contact their customer service department to determine if prior authorization is necessary.
CountyCare Prior Authorization Guidelines
CountyCare provides guidelines for prior authorization, which include:
- Services that require prior authorization
- Medications that require prior authorization
- Exceptions to prior authorization requirements
Step 2: Gather Required Information

To complete the prior authorization form, you'll need to gather specific information, including:
- Patient demographics
- Medical history
- Current treatment plan
- Proposed treatment or service
Required Documents
You may need to submit supporting documentation, such as:
- Medical records
- Test results
- Imaging studies
Step 3: Complete the Prior Authorization Form

The prior authorization form can be completed online or by phone. Ensure that you provide accurate and complete information to avoid delays or denials.
Form Requirements
The prior authorization form requires:
- Patient information
- Service or medication information
- Clinical justification for the request
Step 4: Submit the Prior Authorization Form

Once the form is complete, submit it to CountyCare for review. You can submit the form online, by phone, or by fax.
Submission Guidelines
- Ensure that the form is complete and accurate
- Submit the form within the required timeframe
- Retain a copy of the submitted form for your records
Step 5: Receive a Determination

CountyCare will review the prior authorization form and make a determination. You'll receive notification of the determination, which may include:
- Approval
- Denial
- Request for additional information
Next Steps
If the request is approved, you can proceed with providing the service or prescribing the medication. If the request is denied, you can appeal the decision or request additional information.
By following these 5 easy steps, you can navigate the CountyCare prior authorization process efficiently and effectively. Remember to stay up-to-date with CountyCare's guidelines and policies to ensure a smooth prior authorization process.
We hope this article has provided valuable insights into the CountyCare prior authorization process. If you have any questions or concerns, please don't hesitate to comment below. Share this article with your colleagues and friends to help them understand the prior authorization process.
What is CountyCare prior authorization?
+CountyCare prior authorization is a process that requires healthcare providers to obtain approval from CountyCare before providing certain medical services or prescribing specific medications to patients.
How do I determine if prior authorization is required?
+You can check the CountyCare website or contact their customer service department to determine if prior authorization is necessary.
What information do I need to gather for the prior authorization form?
+You'll need to gather patient demographics, medical history, current treatment plan, and proposed treatment or service.