Accurate and timely submission of CMS Medicare forms is crucial for healthcare providers, medical suppliers, and beneficiaries alike. However, the complexity of these forms can often lead to errors, delays, and even denied claims. In this article, we will delve into the essential tips for filling CMS Medicare forms, ensuring a seamless and efficient process for all parties involved.
As the primary payer for millions of Americans, Medicare plays a vital role in the country's healthcare system. The Centers for Medicare and Medicaid Services (CMS) is responsible for administering Medicare, Medicaid, and the Children's Health Insurance Program (CHIP). With the increasing demand for healthcare services, the importance of accurate and efficient claims processing cannot be overstated. By understanding the intricacies of CMS Medicare forms, healthcare providers can minimize errors, reduce administrative burdens, and ensure timely reimbursement.

In this article, we will explore the essential tips for filling CMS Medicare forms, including understanding the different types of forms, gathering required information, and ensuring accuracy and completeness. Whether you are a healthcare provider, medical supplier, or beneficiary, mastering the art of filling CMS Medicare forms is crucial for a smooth and efficient claims process.
Tip 1: Understand the Different Types of CMS Medicare Forms
CMS Medicare forms come in various shapes and sizes, each serving a specific purpose. The most commonly used forms include:
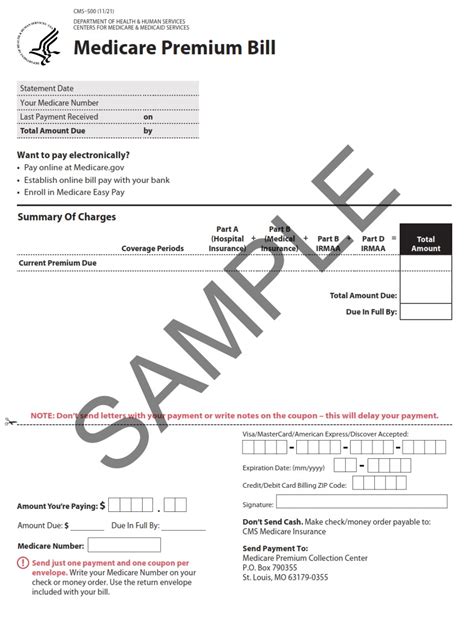
- CMS-1500: Also known as the Health Insurance Claim Form, this is the standard form used by healthcare providers to submit claims for Medicare Part B services.
- CMS-1450: Also known as the Uniform Bill (UB-04), this form is used by hospitals and other healthcare facilities to submit claims for Medicare Part A services.
- CMS-1490S: This form is used by beneficiaries to request reimbursement for Medicare-covered services.
Understanding the different types of CMS Medicare forms is essential to ensure that you are using the correct form for your specific needs.

Tip 2: Gather Required Information Before Filling Out the Form
Before filling out a CMS Medicare form, it is essential to gather all required information. This includes:
- Patient information: Name, date of birth, Medicare ID number, and contact information.
- Provider information: Name, address, and National Provider Identifier (NPI) number.
- Service information: Date of service, type of service, and charges.
- Insurance information: Medicare ID number, coverage dates, and policy number.
Having all required information readily available will save time and reduce errors when filling out the form.
Benefits of Gathering Required Information
- Reduces errors and omissions
- Saves time and increases efficiency
- Ensures accurate and complete claims submission
Tip 3: Ensure Accuracy and Completeness When Filling Out the Form
Accuracy and completeness are crucial when filling out CMS Medicare forms. A single error or omission can lead to delayed or denied claims. To ensure accuracy and completeness:
- Use clear and legible handwriting: Avoid using abbreviations or symbols that may be misinterpreted.
- Use the correct codes and modifiers: Ensure that you are using the correct ICD-10 and CPT codes, as well as any required modifiers.
- Double-check patient and provider information: Verify that patient and provider information is accurate and complete.

Tip 4: Use the Correct Codes and Modifiers
Using the correct codes and modifiers is essential when filling out CMS Medicare forms. This includes:
- ICD-10 codes: Use the correct ICD-10 codes to describe the patient's diagnosis and treatment.
- CPT codes: Use the correct CPT codes to describe the services provided.
- Modifiers: Use required modifiers to describe the services provided, such as the type of service or the location of the service.
Using the correct codes and modifiers ensures that your claims are processed accurately and efficiently.
Benefits of Using Correct Codes and Modifiers
- Ensures accurate and efficient claims processing
- Reduces errors and omissions
- Increases reimbursement accuracy
Tip 5: Verify Form Completion and Submit Correctly
Verifying form completion and submitting correctly is the final step in the process. To ensure that your form is complete and accurate:
- Review the form for errors and omissions: Verify that all required information is complete and accurate.
- Use the correct submission method: Submit the form via the correct method, such as mail or electronic submission.
- Keep a copy of the form: Keep a copy of the form for your records.

By following these essential tips, healthcare providers, medical suppliers, and beneficiaries can ensure a smooth and efficient claims process. Remember to understand the different types of CMS Medicare forms, gather required information, ensure accuracy and completeness, use correct codes and modifiers, and verify form completion and submit correctly.
We encourage you to share your experiences and tips for filling CMS Medicare forms in the comments section below. Your feedback is invaluable in helping us improve our content and provide better resources for our readers.
If you have any questions or need further clarification on any of the topics discussed in this article, please do not hesitate to reach out to us. We are here to help and provide support.
What is the most common type of CMS Medicare form?
+The most common type of CMS Medicare form is the CMS-1500, also known as the Health Insurance Claim Form.
What information is required to fill out a CMS Medicare form?
+Required information includes patient information, provider information, service information, and insurance information.
How can I ensure accuracy and completeness when filling out a CMS Medicare form?
+Use clear and legible handwriting, use the correct codes and modifiers, and double-check patient and provider information.