If you've recently received a denial or reduction of benefits from Cigna, you may be wondering what steps to take next. Fortunately, Cigna offers a reconsideration process that allows you to appeal their decision. In this article, we'll provide a step-by-step guide on how to navigate the Cigna reconsideration form and process.
Receiving a denial of benefits can be a stressful and overwhelming experience, especially if you're dealing with a serious medical condition. However, it's essential to remember that a denial is not the final word. Many insurance companies, including Cigna, have an appeals process in place to ensure that their decisions are fair and accurate.

Understanding the Cigna Reconsideration Process
The Cigna reconsideration process is designed to review and re-evaluate the decision made by the insurance company. This process allows you to provide additional information or evidence that may have been missed during the initial review.
Who Can File an Appeal?
You can file an appeal if:
- You're a Cigna policyholder or beneficiary
- You've received a denial or reduction of benefits
- You disagree with the decision made by Cigna
Step 1: Review Your Denial Letter
Before starting the appeal process, it's essential to review your denial letter carefully. This letter will provide information on why your claim was denied and what information is needed to support your appeal.

What to Look for in Your Denial Letter:
- The reason for the denial
- The specific policy provision or clause that supports the denial
- Any additional information or documentation required to support your appeal
Step 2: Gather Supporting Documentation
To support your appeal, you'll need to gather relevant documentation and information. This may include:
- Medical records and test results
- Letters from your healthcare provider
- Bills and receipts for medical expenses
- Any other relevant documentation that supports your claim
Tips for Gathering Supporting Documentation:
- Make sure to keep detailed records of your medical expenses and treatment
- Request letters from your healthcare provider to support your claim
- Keep all documentation organized and easily accessible
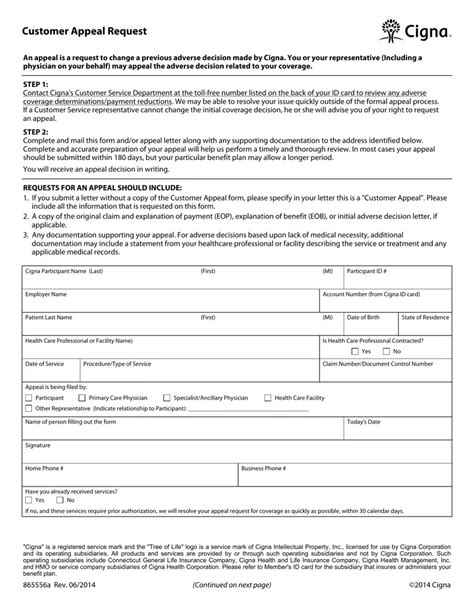
Step 3: Complete the Cigna Reconsideration Form
Once you've gathered all necessary documentation, you can complete the Cigna reconsideration form. This form will require you to provide detailed information about your claim and the reason for your appeal.

What to Include in Your Reconsideration Form:
- A clear explanation of why you're appealing the decision
- A detailed description of your medical condition and treatment
- Any relevant documentation or evidence to support your claim
Step 4: Submit Your Appeal
Once you've completed the reconsideration form and gathered all necessary documentation, you can submit your appeal to Cigna. Make sure to follow the instructions provided by Cigna for submitting your appeal.
Submission Options:
- Mail: Send your appeal to the address provided by Cigna
- Fax: Fax your appeal to the number provided by Cigna
- Online: Submit your appeal through Cigna's online portal
What to Expect After Submitting Your Appeal
After submitting your appeal, Cigna will review your case and make a decision. This process can take several weeks or even months, depending on the complexity of your case.
Next Steps:
- Cigna will review your appeal and make a decision
- You'll receive a letter or notification with the outcome of your appeal
- If your appeal is approved, Cigna will provide information on the next steps to take
Conclusion
The Cigna reconsideration process can be a complex and overwhelming experience. However, by following these steps and gathering the necessary documentation, you can increase your chances of a successful appeal. Remember to stay organized, persistent, and patient throughout the process.

We hope this guide has been helpful in navigating the Cigna reconsideration form and process. If you have any questions or concerns, please don't hesitate to reach out to Cigna or a licensed insurance professional.
What is the Cigna reconsideration process?
+The Cigna reconsideration process is a review of the decision made by Cigna to deny or reduce benefits. This process allows you to provide additional information or evidence to support your claim.
How long does the Cigna reconsideration process take?
+The length of time for the Cigna reconsideration process can vary depending on the complexity of your case. It can take several weeks or even months for Cigna to review your appeal and make a decision.
What documentation do I need to support my appeal?
+You'll need to gather relevant documentation and information to support your appeal, including medical records, letters from your healthcare provider, bills and receipts for medical expenses, and any other relevant documentation that supports your claim.
We encourage you to share your experiences or ask questions about the Cigna reconsideration form and process in the comments section below.