Understanding the nuances of healthcare insurance can be overwhelming, especially when it comes to navigating the complexities of prior authorization. Capital District Physicians' Health Plan (CDPHP) is one such health insurance provider that requires prior authorization for certain medical treatments or procedures. In this article, we will break down the CDPHP prior authorization form process into 5 easy steps, making it simpler for patients and healthcare providers to understand and complete the necessary paperwork.
The Importance of Prior Authorization
Prior authorization is a critical process in healthcare that ensures patients receive necessary medical treatments while also controlling healthcare costs. By requiring prior authorization, insurance providers like CDPHP can verify the medical necessity of a treatment or procedure, reducing the risk of unnecessary or excessive healthcare utilization.

Step 1: Determine if Prior Authorization is Required
The first step in the prior authorization process is to determine if prior authorization is required for a specific treatment or procedure. CDPHP provides a list of services that require prior authorization on their website. Healthcare providers can also contact CDPHP directly to confirm if prior authorization is necessary.
What Services Require Prior Authorization?
CDPHP requires prior authorization for various medical services, including:
- Hospital admissions
- Surgical procedures
- High-cost medications
- Advanced imaging services (e.g., MRI, CT scans)
- Durable medical equipment (DME)
Step 2: Gather Required Information
Once it is determined that prior authorization is required, the next step is to gather the necessary information. This includes:
- Patient demographics (e.g., name, date of birth, policy number)
- Medical history and current diagnosis
- Treatment or procedure details (e.g., CPT code, ICD-10 code)
- Healthcare provider information (e.g., name, contact details)

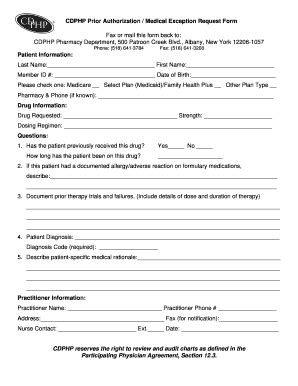
Step 3: Complete the Prior Authorization Form
The prior authorization form can be obtained from the CDPHP website or by contacting CDPHP directly. The form must be completed accurately and thoroughly, including all required information. The form typically includes:
- Patient information
- Medical history and current diagnosis
- Treatment or procedure details
- Healthcare provider information
- Supporting documentation (e.g., medical records, test results)
Tips for Completing the Prior Authorization Form
- Ensure all information is accurate and complete
- Attach supporting documentation as required
- Use a clear and concise writing style
- Sign and date the form
Step 4: Submit the Prior Authorization Form
Once the prior authorization form is complete, it must be submitted to CDPHP for review. The form can be submitted via:
- Fax: (insert fax number)
- Email: (insert email address)
- Online portal: (insert online portal URL)

Step 5: Receive a Determination
After submitting the prior authorization form, CDPHP will review the request and make a determination. The determination will be communicated to the healthcare provider and patient, indicating whether the treatment or procedure is approved or denied.
What to Expect After Submitting the Prior Authorization Form
- A determination will be made within a specified timeframe (e.g., 3-5 business days)
- The determination will be communicated via phone, email, or mail
- If approved, the patient can proceed with the treatment or procedure
- If denied, the patient or healthcare provider can appeal the decision
By following these 5 easy steps, patients and healthcare providers can navigate the CDHP prior authorization form process with ease. Remember to stay organized, gather required information, and complete the form accurately to ensure a smooth and efficient process.
We hope this article has provided valuable insights into the CDHP prior authorization form process. If you have any questions or concerns, please feel free to comment below.
What is prior authorization?
+Prior authorization is a process where a healthcare insurance provider reviews a patient's medical treatment or procedure to determine if it is medically necessary.
How long does the prior authorization process take?
+The prior authorization process typically takes 3-5 business days, but this timeframe may vary depending on the insurance provider and the complexity of the request.