Caresource is a leading health insurance provider that offers a range of plans to individuals, families, and employers. One of the essential aspects of Caresource's healthcare services is the prior authorization process. This process ensures that patients receive necessary medical treatments while also controlling healthcare costs. In this article, we will delve into the Caresource prior authorization form, its importance, and provide a step-by-step guide on how to complete it.

The prior authorization process is a critical step in ensuring that patients receive the necessary medical treatments while also controlling healthcare costs. It involves submitting a request to Caresource for approval before a patient undergoes a specific medical treatment or procedure. This process helps to ensure that the treatment is medically necessary and aligns with Caresource's coverage policies.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- Cost Control: Prior authorization helps to control healthcare costs by ensuring that medical treatments are medically necessary and align with Caresource's coverage policies.
- Improved Patient Outcomes: Prior authorization ensures that patients receive the most effective and safe medical treatments, which can lead to improved patient outcomes.
- Reduced Administrative Burden: Prior authorization can help reduce administrative burdens on healthcare providers by streamlining the approval process.
How to Complete the Caresource Prior Authorization Form
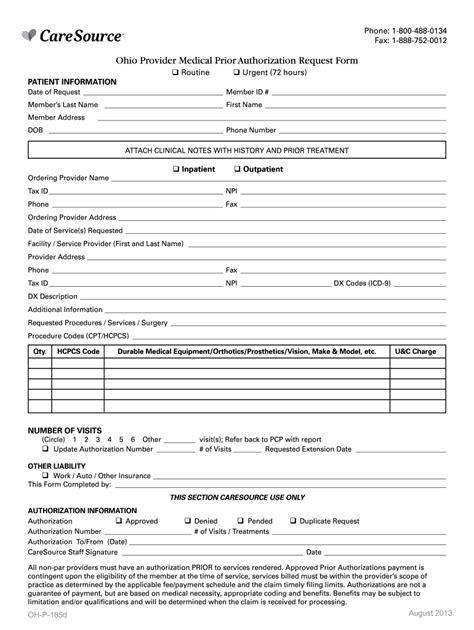
Completing the Caresource prior authorization form requires careful attention to detail and a thorough understanding of the patient's medical condition and treatment plan. Here is a step-by-step guide to help you complete the form:
Step 1: Gather Required Information
Before starting the prior authorization process, gather the following information:
- Patient's name and date of birth
- Patient's Caresource membership ID
- Description of the medical treatment or procedure
- Diagnosis code(s) and procedure code(s)
- Healthcare provider's name and contact information

Step 2: Complete the Prior Authorization Form
The Caresource prior authorization form is typically completed by the healthcare provider or their authorized representative. The form requires the following information:
- Patient's demographic information
- Medical treatment or procedure description
- Diagnosis code(s) and procedure code(s)
- Healthcare provider's signature and contact information
Step 3: Submit the Prior Authorization Form
Once the prior authorization form is complete, submit it to Caresource for review. The form can be submitted via fax, email, or online portal.
Caresource Prior Authorization Form Requirements
To ensure a smooth prior authorization process, the following requirements must be met:
- Complete and Accurate Information: The prior authorization form must be complete and accurate to avoid delays or denials.
- Required Documentation: Supporting documentation, such as medical records and test results, may be required to support the prior authorization request.
- Timely Submission: The prior authorization form must be submitted in a timely manner to avoid delays in treatment.

Caresource Prior Authorization FAQs
Here are some frequently asked questions about the Caresource prior authorization process:
Q: What is the turnaround time for prior authorization requests?
A: The turnaround time for prior authorization requests varies depending on the type of request and the complexity of the case. Standard requests are typically processed within 3-5 business days, while expedited requests are processed within 24 hours.
Q: Can I submit prior authorization requests online?
A: Yes, Caresource offers an online portal for submitting prior authorization requests. Healthcare providers can register for an account and submit requests electronically.
Q: What if my prior authorization request is denied?
A: If a prior authorization request is denied, the healthcare provider or patient can appeal the decision. The appeal process typically involves submitting additional information or documentation to support the request.
What is the Caresource prior authorization phone number?
+The Caresource prior authorization phone number is 1-800-479-2149.
Can I submit prior authorization requests via fax?
+What is the Caresource prior authorization email address?
+The Caresource prior authorization email address is .
In conclusion, the Caresource prior authorization form is an essential tool for ensuring that patients receive necessary medical treatments while controlling healthcare costs. By following the step-by-step guide outlined in this article, healthcare providers can ensure a smooth prior authorization process and reduce administrative burdens. We encourage you to share your experiences with the Caresource prior authorization process in the comments section below.