In the ever-evolving landscape of healthcare, efficient management of prescriptions and medical treatments is crucial. For those enrolled in the Caremark Federal Employee Program (FEP), understanding the process of prior authorization is essential. Prior authorization is a requirement for certain medications and treatments, ensuring that patients receive the most effective and safe care while also managing healthcare costs. One of the critical documents in this process is the Caremark FEP Prior Authorization Form. Completing this form accurately and efficiently can expedite the approval process, minimizing delays in accessing necessary medications or treatments. Here's a step-by-step guide on how to complete the Caremark FEP Prior Authorization Form:

Understanding the Caremark FEP Prior Authorization Process
Before diving into the steps to complete the form, it's essential to understand the purpose and scope of the prior authorization process. Prior authorization is a process used by health insurance companies to determine if a prescribed medication or treatment is medically necessary and covered under the patient's insurance plan. This process aims to ensure that patients receive appropriate and cost-effective care.
Why is Prior Authorization Important?
Prior authorization plays a critical role in healthcare management for several reasons:
- Ensures Safety and Efficacy: It helps ensure that patients receive medications or treatments that are safe and effective for their specific condition.
- Reduces Healthcare Costs: By reviewing the medical necessity of certain treatments or medications, prior authorization helps manage healthcare costs and prevent unnecessary expenses.
- Improves Patient Outcomes: By ensuring that patients receive the most appropriate care, prior authorization can lead to better health outcomes.
Step 1: Gather Necessary Information

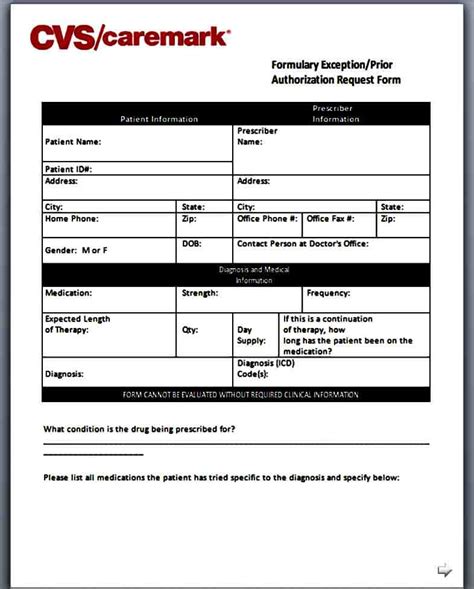
The first step in completing the Caremark FEP Prior Authorization Form is to gather all the necessary information. This includes:
- Patient Information: Full name, date of birth, and contact information.
- Prescription Details: The name of the medication, dosage, frequency, and duration of treatment.
- Clinical Information: Diagnosis, medical history relevant to the current treatment, and any previous treatments or medications tried.
- Physician Information: The prescribing physician's name, contact information, and medical license number.
Importance of Accurate Information
Accurate and complete information is crucial for a successful prior authorization process. Incomplete or incorrect information can lead to delays or even denials of the prior authorization request.
Step 2: Choose the Correct Form

Caremark provides different forms for various types of prior authorizations. It's essential to choose the correct form that matches the type of medication or treatment being requested. Forms can usually be found on the Caremark FEP website or by contacting their customer service.
Types of Forms
- Medication Prior Authorization Form: For requesting approval for specific medications.
- Treatment Prior Authorization Form: For requesting approval for certain medical treatments or procedures.
Step 3: Fill Out the Form

Once you have the correct form and all the necessary information, the next step is to fill it out accurately and completely. Make sure to follow these tips:
- Read Instructions Carefully: Understand what information is required and how it should be presented.
- Use Clear and Legible Writing: Ensure that all information is easy to read and understand.
- Do Not Leave Blank Spaces: Provide all required information. If a section does not apply, indicate that with "N/A" or "Not Applicable."
Tips for a Smooth Process
- Use the Correct Codes: Use the correct medication codes or treatment codes as required by the form.
- Include Supporting Documents: Attach any supporting medical documents or records as requested.
Step 4: Submit the Form

After completing the form, the next step is to submit it to Caremark FEP. Forms can usually be submitted online, by fax, or by mail, depending on the instructions provided by Caremark. Ensure you keep a copy of the submitted form for your records.
Methods of Submission
- Online Submission: Through the Caremark FEP website or portal.
- Fax Submission: By sending the form to the fax number provided by Caremark.
- Mail Submission: By sending the form to the address provided by Caremark.
Step 5: Follow Up on Your Request

After submitting the form, it's essential to follow up on your prior authorization request. This can be done by contacting Caremark FEP's customer service or checking the status online through their portal.
Importance of Follow-Up
Following up ensures that the process moves forward smoothly and that any issues are addressed promptly. It also gives you the opportunity to provide any additional information that might be required.
Conclusion and Next Steps
Completing the Caremark FEP Prior Authorization Form is a straightforward process when you have the right information and follow the correct steps. By understanding the importance of prior authorization, gathering necessary information, choosing the correct form, filling it out accurately, submitting it properly, and following up on your request, you can ensure a smooth and efficient process.

For further assistance or to clarify any doubts, don't hesitate to reach out to Caremark FEP's customer service. They are there to help you navigate the process and answer any questions you might have.
We invite you to share your experiences or ask any questions you might have about the Caremark FEP Prior Authorization Form process in the comments below. Your insights can help others navigate this process more effectively.
What is the purpose of the Caremark FEP Prior Authorization Form?
+The Caremark FEP Prior Authorization Form is used to determine if a prescribed medication or treatment is medically necessary and covered under the patient's insurance plan.
How do I choose the correct Caremark FEP form for prior authorization?
+Forms can be found on the Caremark FEP website, and you should choose the form that matches the type of medication or treatment being requested.
What happens after I submit the Caremark FEP Prior Authorization Form?
+After submitting the form, Caremark FEP will review the request. You should follow up on your request to ensure the process moves forward smoothly and to address any issues promptly.