The world of healthcare can be a complex and daunting place, especially when it comes to dealing with insurance companies and prior authorizations. If you're a healthcare provider or patient looking to navigate the process of filling out a CareFirst prior authorization form, you're in the right place. In this article, we'll break down the process into 5 easy ways to make it more manageable.
CareFirst, one of the largest health insurance companies in the Mid-Atlantic region, requires prior authorization for certain medical procedures and treatments. This process ensures that patients receive necessary and cost-effective care while also protecting the insurance company from unnecessary expenses. However, the prior authorization process can be lengthy and time-consuming, often causing frustration for both healthcare providers and patients.
In this article, we'll explore the 5 easy ways to fill out a CareFirst prior authorization form, making the process more efficient and stress-free.
What is Prior Authorization?

Prior authorization is a process used by health insurance companies to determine whether a particular medical treatment or procedure is medically necessary and covered under the patient's insurance plan. This process typically involves the healthcare provider submitting a request to the insurance company, which then reviews the request and makes a determination.
Prior authorization is often required for:
- High-cost medications
- Surgical procedures
- Hospital admissions
- Advanced imaging tests (e.g., MRI, CT scans)
Why is Prior Authorization Important?
Prior authorization plays a crucial role in ensuring that patients receive necessary and cost-effective care. By reviewing medical requests before treatment, insurance companies can:
- Ensure that patients receive evidence-based care
- Reduce unnecessary medical expenses
- Prevent overutilization of healthcare services
- Improve patient outcomes
Benefits of Prior Authorization
While prior authorization can be time-consuming, it offers several benefits, including:
- Reduced healthcare costs
- Improved patient safety
- Enhanced quality of care
- Reduced risk of medical errors
5 Easy Ways to Fill Out a CareFirst Prior Authorization Form
Now that we've covered the basics of prior authorization, let's dive into the 5 easy ways to fill out a CareFirst prior authorization form.
1. Gather Required Information
Before starting the prior authorization process, gather all required information, including:
- Patient demographics
- Medical history
- Current medications
- Proposed treatment or procedure
- Supporting medical documentation (e.g., test results, medical records)

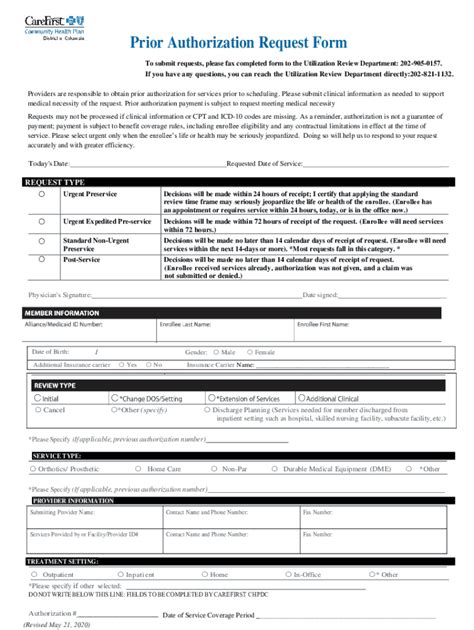
2. Choose the Right Form
CareFirst offers various prior authorization forms, each designed for specific medical services or procedures. Ensure you choose the correct form for the requested treatment or procedure.
- Review the CareFirst website for the most up-to-date forms
- Contact CareFirst customer service for assistance
3. Complete the Form Accurately
Complete the prior authorization form accurately and thoroughly, ensuring all required information is included.
- Use clear and concise language
- Avoid abbreviations and jargon
- Include supporting medical documentation

4. Submit the Form Electronically
CareFirst offers electronic submission options for prior authorization forms, making the process faster and more efficient.
- Use the CareFirst online portal to submit forms
- Ensure all required information is included
5. Follow Up on the Status
After submitting the prior authorization form, follow up on the status to ensure timely processing.
- Contact CareFirst customer service for updates
- Use the CareFirst online portal to track the status

Additional Tips and Reminders
To ensure a smooth prior authorization process, keep the following tips and reminders in mind:
- Submit prior authorization requests well in advance of the proposed treatment or procedure
- Ensure all required information is included to avoid delays
- Follow up on the status regularly to ensure timely processing
Conclusion: Streamlining the Prior Authorization Process
Filling out a CareFirst prior authorization form can be a daunting task, but by following these 5 easy ways, you can make the process more efficient and stress-free. Remember to gather required information, choose the right form, complete the form accurately, submit the form electronically, and follow up on the status.
By streamlining the prior authorization process, you can reduce delays, improve patient outcomes, and enhance the overall quality of care.

Now it's your turn! Share your experiences and tips for navigating the prior authorization process in the comments below.
FAQ Section:
What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a particular medical treatment or procedure is medically necessary and covered under the patient's insurance plan.
Why is prior authorization important?
+Prior authorization is important because it ensures that patients receive necessary and cost-effective care, reduces unnecessary medical expenses, and prevents overutilization of healthcare services.
How do I submit a prior authorization request to CareFirst?
+You can submit a prior authorization request to CareFirst through their online portal or by contacting their customer service department.