Prior authorization for medication can be a daunting and time-consuming process for healthcare providers, patients, and pharmacists alike. CareFirst, a leading health insurance provider, requires prior authorization for certain medications to ensure that patients receive necessary and cost-effective treatments. However, this process can be complex and may lead to delays in treatment. In this article, we will discuss five ways to simplify the CareFirst prior authorization process for medication.
The prior authorization process involves several steps, including submitting a request to CareFirst, providing medical records and supporting documentation, and waiting for a decision. This process can be overwhelming, especially for healthcare providers who need to manage multiple patients and requests simultaneously. Moreover, delays in prior authorization can lead to treatment delays, which can negatively impact patient health outcomes.
Fortunately, there are ways to simplify the CareFirst prior authorization process for medication. By implementing these strategies, healthcare providers, patients, and pharmacists can reduce the administrative burden and ensure that patients receive timely access to necessary medications.
Streamline Your Workflow with Electronic Prior Authorization

One way to simplify the prior authorization process is by using electronic prior authorization (ePA) systems. ePA systems allow healthcare providers to submit prior authorization requests electronically, reducing paperwork and administrative burdens. These systems can also automate the process, ensuring that all necessary information is included and reducing the risk of errors.
CareFirst offers an ePA system that allows healthcare providers to submit prior authorization requests online. This system provides a streamlined and efficient way to manage prior authorization requests, reducing the time and effort required to complete the process.
Benefits of Electronic Prior Authorization
- Reduces paperwork and administrative burdens
- Automates the process, reducing errors and increasing efficiency
- Allows for real-time tracking and updates on prior authorization requests
- Enhances patient care by reducing treatment delays
Use a Prior Authorization Tool to Automate the Process

Another way to simplify the prior authorization process is by using a prior authorization tool. These tools can automate the process, ensuring that all necessary information is included and reducing the risk of errors. Prior authorization tools can also provide real-time tracking and updates on prior authorization requests, enhancing patient care and reducing treatment delays.
CareFirst offers a prior authorization tool that allows healthcare providers to automate the prior authorization process. This tool provides a user-friendly interface, allowing healthcare providers to easily submit prior authorization requests and track the status of their requests.
Benefits of Prior Authorization Tools
- Automates the prior authorization process, reducing errors and increasing efficiency
- Provides real-time tracking and updates on prior authorization requests
- Enhances patient care by reducing treatment delays
- Reduces administrative burdens, allowing healthcare providers to focus on patient care
Verify Patient Eligibility and Benefits Before Submitting a Prior Authorization Request

Verifying patient eligibility and benefits before submitting a prior authorization request can help simplify the process. This step ensures that the patient is eligible for coverage and that the medication is covered under their plan. By verifying eligibility and benefits upfront, healthcare providers can avoid delays and reduce the risk of prior authorization requests being denied.
CareFirst provides an online tool that allows healthcare providers to verify patient eligibility and benefits. This tool provides real-time information, ensuring that healthcare providers have the most up-to-date information on patient eligibility and benefits.
Benefits of Verifying Patient Eligibility and Benefits
- Reduces the risk of prior authorization requests being denied
- Ensures that patients are eligible for coverage and that medications are covered under their plan
- Reduces administrative burdens, allowing healthcare providers to focus on patient care
- Enhances patient care by reducing treatment delays
Provide Complete and Accurate Information When Submitting a Prior Authorization Request

Providing complete and accurate information when submitting a prior authorization request is crucial to simplifying the process. This includes providing all necessary medical records and supporting documentation, as well as ensuring that the request is complete and accurate.
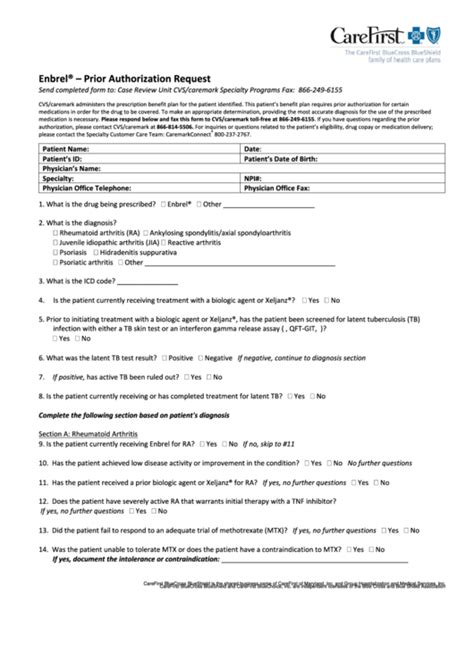
CareFirst provides a checklist of required information for prior authorization requests. This checklist ensures that healthcare providers provide all necessary information, reducing the risk of delays and denials.
Benefits of Providing Complete and Accurate Information
- Reduces the risk of delays and denials
- Ensures that prior authorization requests are processed efficiently
- Enhances patient care by reducing treatment delays
- Reduces administrative burdens, allowing healthcare providers to focus on patient care
Follow Up on Prior Authorization Requests to Ensure Timely Processing

Finally, following up on prior authorization requests is essential to ensuring timely processing. This involves tracking the status of prior authorization requests and following up with CareFirst to ensure that requests are processed efficiently.
CareFirst provides a online tool that allows healthcare providers to track the status of prior authorization requests. This tool provides real-time information, ensuring that healthcare providers have the most up-to-date information on the status of prior authorization requests.
Benefits of Following Up on Prior Authorization Requests
- Ensures timely processing of prior authorization requests
- Reduces the risk of delays and denials
- Enhances patient care by reducing treatment delays
- Reduces administrative burdens, allowing healthcare providers to focus on patient care
In conclusion, simplifying the CareFirst prior authorization process for medication requires a combination of strategies. By implementing these strategies, healthcare providers, patients, and pharmacists can reduce the administrative burden and ensure that patients receive timely access to necessary medications.
We invite you to share your thoughts and experiences on simplifying the prior authorization process. Have you used any of the strategies mentioned in this article? What challenges have you faced, and how have you overcome them? Share your comments below and let's continue the conversation.
What is prior authorization, and why is it required?
+Prior authorization is a process required by health insurance providers to ensure that patients receive necessary and cost-effective treatments. It involves submitting a request to the health insurance provider, providing medical records and supporting documentation, and waiting for a decision.
How long does the prior authorization process take?
+The prior authorization process can take several days to several weeks, depending on the complexity of the request and the efficiency of the health insurance provider's processing system.
What can I do to simplify the prior authorization process?
+You can simplify the prior authorization process by using electronic prior authorization systems, prior authorization tools, verifying patient eligibility and benefits, providing complete and accurate information, and following up on prior authorization requests.