As a healthcare provider, you understand the importance of ensuring that your patients receive the necessary medical treatments and services. However, navigating the prior authorization process can be complex and time-consuming. In this article, we will guide you through the Brown & Toland prior authorization form process, breaking it down into 5 easy steps.
What is Prior Authorization and Why is it Necessary?
Prior authorization, also known as pre-authorization or pre-certification, is a process required by some health insurance providers, including Brown & Toland, to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan. This process is in place to ensure that patients receive high-quality, cost-effective care, while also minimizing unnecessary medical expenses.

Benefits of Prior Authorization
While prior authorization may seem like an additional administrative burden, it offers several benefits to both patients and healthcare providers. Some of these benefits include:
- Reduced healthcare costs by minimizing unnecessary treatments and services
- Improved patient outcomes by ensuring that patients receive medically necessary care
- Enhanced care coordination and communication between healthcare providers and insurance companies
- Streamlined billing and reimbursement processes
Common Services Requiring Prior Authorization
The following services typically require prior authorization from Brown & Toland:
- Inpatient hospital admissions
- Outpatient surgeries and procedures
- Chemotherapy and radiation therapy
- Imaging services (e.g., MRI, CT scans)
- Prescription medications (e.g., specialty medications, injectables)
Step 1: Check Patient Eligibility
Before starting the prior authorization process, verify the patient's eligibility for benefits under their Brown & Toland insurance plan. You can do this by:
- Checking the patient's insurance card or identification
- Contacting Brown & Toland's customer service department
- Using Brown & Toland's online portal or eligibility verification tool

Step 2: Gather Required Information
To complete the prior authorization form, you will need to gather the following information:
- Patient demographics and insurance information
- Diagnosis and medical condition
- Proposed treatment or service
- Supporting medical documentation (e.g., test results, medical records)
Required Documents
The following documents may be required to support the prior authorization request:
- Medical records and test results
- Prescription information
- Treatment plans and proposals
- Letters of medical necessity
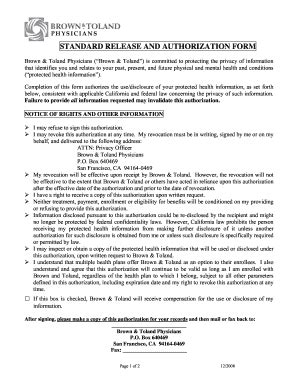
Step 3: Complete the Prior Authorization Form
The Brown & Toland prior authorization form can be completed online or by phone. You can:
- Access the online form through Brown & Toland's provider portal
- Contact Brown & Toland's prior authorization department by phone
- Fax the completed form to Brown & Toland's prior authorization department

Step 4: Submit the Prior Authorization Request
Once you have completed the prior authorization form, submit it to Brown & Toland for review. You can:
- Fax the completed form to Brown & Toland's prior authorization department
- Upload the form through Brown & Toland's provider portal
- Mail the form to Brown & Toland's prior authorization department
Timeline for Prior Authorization
Brown & Toland typically reviews prior authorization requests within 24-48 hours. However, this timeline may vary depending on the complexity of the request and the availability of medical records.
Step 5: Follow Up on the Prior Authorization Request
After submitting the prior authorization request, follow up with Brown & Toland to confirm receipt and status. You can:
- Contact Brown & Toland's prior authorization department by phone
- Check the status of the request through Brown & Toland's provider portal
- Respond to any additional information requests from Brown & Toland

By following these 5 easy steps, you can ensure a smooth prior authorization process for your patients. Remember to check patient eligibility, gather required information, complete the prior authorization form, submit the request, and follow up on the status.
We hope this article has provided valuable insights into the Brown & Toland prior authorization form process. If you have any questions or concerns, please don't hesitate to comment below. Share this article with your colleagues and peers to help streamline the prior authorization process.
What is prior authorization?
+Prior authorization is a process required by some health insurance providers to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan.
How long does the prior authorization process take?
+Brown & Toland typically reviews prior authorization requests within 24-48 hours. However, this timeline may vary depending on the complexity of the request and the availability of medical records.
What documents are required to support the prior authorization request?
+The following documents may be required to support the prior authorization request: medical records and test results, prescription information, treatment plans and proposals, and letters of medical necessity.