As a healthcare provider in Michigan, navigating the prior authorization process for Blue Cross Blue Shield (BCBS) can be a daunting task. Prior authorization, also known as pre-certification or pre-authorization, is a process used by health insurance companies to determine whether a specific treatment or service is medically necessary and covered under a patient's insurance plan. In this article, we will guide you through the Michigan BCBS prior authorization form process, providing you with the information you need to ensure a smooth and efficient experience for your patients.
Understanding the Importance of Prior Authorization
Prior authorization is a crucial step in the healthcare process, as it ensures that patients receive necessary and appropriate care while also controlling healthcare costs. By requiring prior authorization, BCBS can review the medical necessity of a treatment or service before it is rendered, reducing the likelihood of denied claims and unnecessary procedures. As a healthcare provider, it is essential to understand the prior authorization process to avoid delays or denials of care for your patients.
Michigan BCBS Prior Authorization Form: What You Need to Know
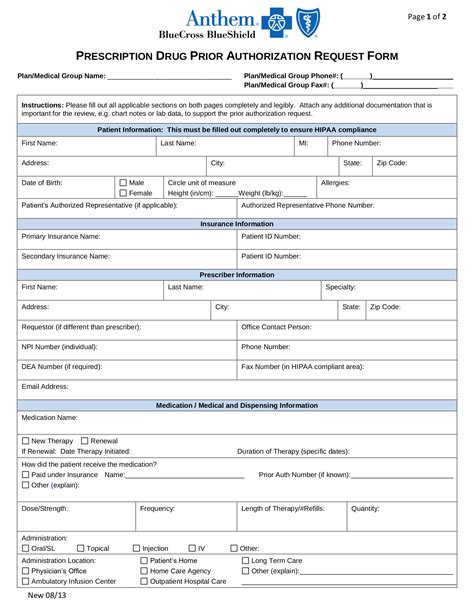
The Michigan BCBS prior authorization form is used to request approval for various medical services, including prescriptions, surgeries, and diagnostic tests. The form requires specific information about the patient, the treatment or service being requested, and the medical justification for the request. Here are some key things to keep in mind when completing the Michigan BCBS prior authorization form:

- Patient Information: Include the patient's name, date of birth, and BCBS member ID number.
- Treatment or Service: Clearly describe the treatment or service being requested, including the CPT code and dosage (if applicable).
- Medical Justification: Provide a detailed explanation of the medical necessity of the treatment or service, including relevant medical history and current symptoms.
- Supporting Documentation: Attach any supporting documentation, such as lab results, medical records, or test results.
How to Submit the Michigan BCBS Prior Authorization Form
Once you have completed the Michigan BCBS prior authorization form, you can submit it to BCBS via various methods, including:
- Online Portal: BCBS offers an online portal for providers to submit prior authorization requests electronically.
- Fax: You can fax the completed form to BCBS at the fax number listed on their website.
- Mail: You can mail the completed form to BCBS at the address listed on their website.
Tips for a Smooth Prior Authorization Process
To ensure a smooth prior authorization process, follow these tips:
- Submit the form completely and accurately: Make sure to include all required information and documentation to avoid delays or denials.
- Use the correct form: Use the most up-to-date version of the Michigan BCBS prior authorization form to avoid rejection.
- Allow sufficient time: Submit the form well in advance of the scheduled treatment or service to allow time for review and approval.
- Follow up: If you haven't received a response from BCBS within the expected timeframe, follow up with a phone call or email to check on the status of your request.
Benefits of Electronic Prior Authorization
Electronic prior authorization (ePA) offers several benefits, including:
- Faster turnaround times: ePA requests are typically reviewed and approved faster than paper-based requests.
- Increased accuracy: ePA reduces the risk of errors and missing information.
- Reduced administrative burden: ePA automates the prior authorization process, reducing the administrative burden on providers.
Common Prior Authorization Form Mistakes to Avoid
Here are some common mistakes to avoid when completing the Michigan BCBS prior authorization form:
- Incomplete or inaccurate information: Make sure to include all required information and documentation.
- Incorrect CPT code: Verify the CPT code to ensure it matches the treatment or service being requested.
- Lack of medical justification: Provide a clear and concise explanation of the medical necessity of the treatment or service.
Conclusion and Next Steps
In conclusion, the Michigan BCBS prior authorization form is an essential tool for healthcare providers to ensure that patients receive necessary and appropriate care while controlling healthcare costs. By following the tips and guidelines outlined in this article, you can ensure a smooth and efficient prior authorization process for your patients. If you have any questions or concerns about the prior authorization process, don't hesitate to reach out to BCBS or a qualified healthcare professional.
We invite you to comment below with any questions or feedback about this article. Share this article with your colleagues and friends to help them navigate the prior authorization process.