The prior authorization process can be a significant burden for healthcare providers, particularly when dealing with Blue Cross Blue Shield (BCBS). The process can be time-consuming, costly, and may delay patient care. However, there are steps that providers can take to simplify the prior authorization process for BCBS.
Understanding the Prior Authorization Process
Before we dive into the steps to simplify the prior authorization process, it's essential to understand how it works. Prior authorization, also known as pre-certification or pre-authorization, is a process where healthcare providers must obtain approval from the patient's insurance provider before performing a specific treatment or procedure. This process is designed to ensure that the treatment is medically necessary and meets the insurance provider's coverage guidelines.
Step 1: Verify Patient Eligibility and Benefits
Verifying patient eligibility and benefits is the first step in simplifying the prior authorization process. This step can help prevent unnecessary prior authorization requests and reduce the risk of denied claims. Providers can use the BCBS website or automated phone system to verify patient eligibility and benefits.

Step 2: Check the BCBS Prior Authorization List
BCBS maintains a list of procedures and treatments that require prior authorization. Providers can check this list to determine if a prior authorization is required for a specific treatment or procedure. This step can help prevent unnecessary prior authorization requests and reduce the risk of denied claims.
Step 3: Use Electronic Prior Authorization
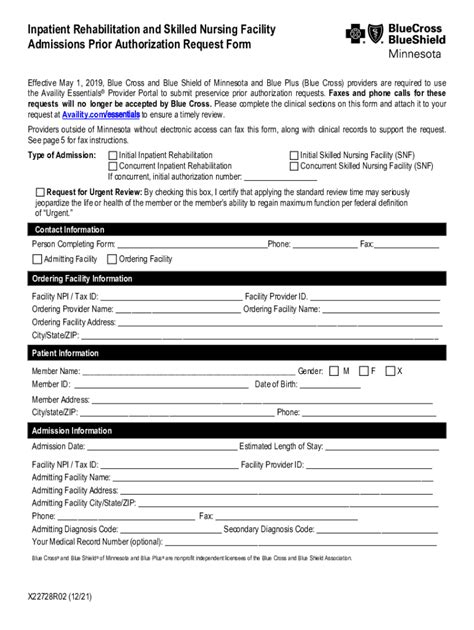
Electronic prior authorization (ePA) is a faster and more efficient way to obtain prior authorization. ePA allows providers to submit prior authorization requests electronically, reducing the need for phone calls and faxes. BCBS offers an ePA system that providers can use to submit prior authorization requests.

Step 4: Ensure Accurate and Complete Documentation
Accurate and complete documentation is essential for a successful prior authorization request. Providers should ensure that all required documentation, including medical records and test results, are submitted with the prior authorization request. Incomplete or inaccurate documentation can lead to delayed or denied prior authorization requests.
Step 5: Follow Up on Prior Authorization Requests
Following up on prior authorization requests is crucial to ensure that the request is processed in a timely manner. Providers can use the BCBS website or automated phone system to check the status of prior authorization requests. This step can help prevent delays in patient care and reduce the risk of denied claims.

Benefits of Simplifying the Prior Authorization Process
Simplifying the prior authorization process can have numerous benefits for healthcare providers, including:
- Reduced administrative burden
- Improved patient satisfaction
- Reduced risk of denied claims
- Faster reimbursement
Tips for Healthcare Providers
Here are some additional tips for healthcare providers to simplify the prior authorization process:
- Use a prior authorization checklist to ensure that all required documentation is submitted
- Designate a staff member to handle prior authorization requests
- Use a prior authorization tracking system to monitor the status of requests
- Educate patients on the prior authorization process and the importance of accurate documentation

Conclusion
Simplifying the prior authorization process can help reduce the administrative burden on healthcare providers and improve patient satisfaction. By following the steps outlined in this article, providers can reduce the risk of denied claims and improve the overall efficiency of the prior authorization process. Remember to verify patient eligibility and benefits, check the BCBS prior authorization list, use electronic prior authorization, ensure accurate and complete documentation, and follow up on prior authorization requests.

FAQs
What is prior authorization?
+Prior authorization, also known as pre-certification or pre-authorization, is a process where healthcare providers must obtain approval from the patient's insurance provider before performing a specific treatment or procedure.
How do I verify patient eligibility and benefits?
+You can verify patient eligibility and benefits using the BCBS website or automated phone system.
What is electronic prior authorization?
+Electronic prior authorization (ePA) is a faster and more efficient way to obtain prior authorization. ePA allows providers to submit prior authorization requests electronically, reducing the need for phone calls and faxes.