Navigating the complexities of healthcare can be overwhelming, especially when it comes to prior authorizations. The BCBS FEP prior authorization form is a crucial document that helps ensure patients receive the necessary medical treatments while also controlling healthcare costs. In this article, we will delve into the world of prior authorizations, explaining what they are, why they're necessary, and providing a step-by-step guide on how to complete the BCBS FEP prior authorization form.
What is a Prior Authorization?
Prior authorization, also known as pre-authorization or pre-certification, is a process used by health insurance companies to determine whether a particular medical treatment or service is medically necessary and covered under the patient's insurance plan. This process helps prevent unnecessary medical procedures, reduce healthcare costs, and ensure that patients receive only the treatments that are medically necessary.
Why is Prior Authorization Necessary?
Prior authorization is necessary for several reasons:
- It helps control healthcare costs by preventing unnecessary medical procedures.
- It ensures that patients receive only the treatments that are medically necessary.
- It helps reduce the risk of adverse reactions or complications from unnecessary treatments.
- It allows health insurance companies to negotiate better rates with healthcare providers.

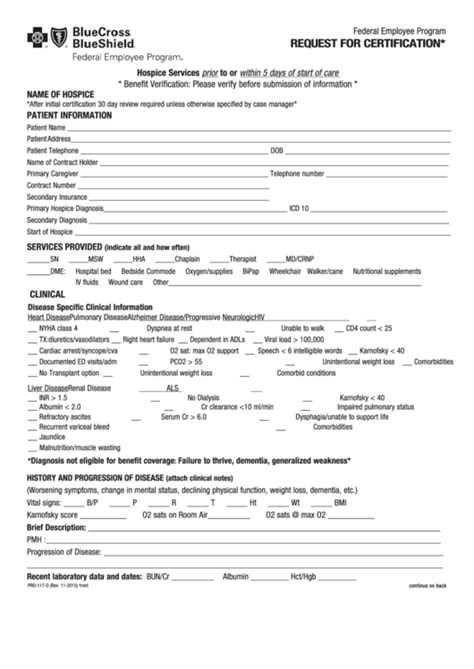
What is the BCBS FEP Prior Authorization Form?
The BCBS FEP prior authorization form is a document used by the Blue Cross Blue Shield Federal Employee Program (BCBS FEP) to request prior authorization for medical treatments or services. The form is typically completed by the patient's healthcare provider and submitted to BCBS FEP for review.
Step-by-Step Guide to Completing the BCBS FEP Prior Authorization Form
Completing the BCBS FEP prior authorization form can be a complex process, but by following these steps, you can ensure that your request is processed efficiently.
Step 1: Gather Required Information
Before completing the form, gather the following information:
- Patient's name and BCBS FEP identification number
- Patient's date of birth and contact information
- Healthcare provider's name and contact information
- Medical treatment or service being requested
- Diagnosis and medical necessity for the treatment or service
Step 2: Complete the Patient Information Section
Complete the patient information section of the form, including the patient's name, BCBS FEP identification number, date of birth, and contact information.
Step 3: Complete the Healthcare Provider Information Section
Complete the healthcare provider information section of the form, including the provider's name and contact information.
Step 4: Describe the Medical Treatment or Service
Describe the medical treatment or service being requested, including the diagnosis and medical necessity for the treatment or service.
Step 5: Attach Supporting Documentation
Attach supporting documentation, such as medical records and test results, to the form.
Step 6: Submit the Form
Submit the completed form to BCBS FEP for review.

Tips for Completing the BCBS FEP Prior Authorization Form
- Ensure that all required information is complete and accurate.
- Attach supporting documentation to the form.
- Submit the form well in advance of the scheduled treatment or service.
- Follow up with BCBS FEP to ensure that the form has been received and is being processed.
Common Mistakes to Avoid
- Incomplete or inaccurate information
- Failure to attach supporting documentation
- Submitting the form too close to the scheduled treatment or service
- Failure to follow up with BCBS FEP

Conclusion
The BCBS FEP prior authorization form is a crucial document that helps ensure patients receive the necessary medical treatments while also controlling healthcare costs. By following the step-by-step guide outlined in this article, you can ensure that your request is processed efficiently. Remember to gather all required information, complete the form accurately, and attach supporting documentation.
FAQs
Q: What is the purpose of the BCBS FEP prior authorization form?
A: The purpose of the BCBS FEP prior authorization form is to request prior authorization for medical treatments or services.
Q: Who completes the BCBS FEP prior authorization form?
A: The BCBS FEP prior authorization form is typically completed by the patient's healthcare provider.
Q: What information is required to complete the BCBS FEP prior authorization form?
A: The required information includes patient's name and BCBS FEP identification number, patient's date of birth and contact information, healthcare provider's name and contact information, medical treatment or service being requested, diagnosis and medical necessity for the treatment or service.
Q: How do I submit the BCBS FEP prior authorization form?
A: The completed form should be submitted to BCBS FEP for review.
Q: How long does it take for BCBS FEP to process the prior authorization form?
A: The processing time may vary depending on the complexity of the request and the availability of information.
What is the purpose of the BCBS FEP prior authorization form?
+The purpose of the BCBS FEP prior authorization form is to request prior authorization for medical treatments or services.
Who completes the BCBS FEP prior authorization form?
+The BCBS FEP prior authorization form is typically completed by the patient's healthcare provider.
What information is required to complete the BCBS FEP prior authorization form?
+The required information includes patient's name and BCBS FEP identification number, patient's date of birth and contact information, healthcare provider's name and contact information, medical treatment or service being requested, diagnosis and medical necessity for the treatment or service.
How do I submit the BCBS FEP prior authorization form?
+The completed form should be submitted to BCBS FEP for review.
How long does it take for BCBS FEP to process the prior authorization form?
+The processing time may vary depending on the complexity of the request and the availability of information.