Understanding the intricacies of health insurance and medical billing can be overwhelming for healthcare providers and patients alike. One crucial aspect of the process is prior authorization, a step that ensures patients receive the necessary treatment while also controlling healthcare costs. In this article, we will delve into the Blue Advantage prior authorization form, its importance, and provide a comprehensive guide on how to master the process.
The Significance of Prior Authorization
Prior authorization is a critical step in the healthcare process that involves obtaining approval from a patient's health insurance provider before proceeding with a specific treatment or medication. This step is essential for several reasons. Firstly, it ensures that patients receive the necessary treatment while also controlling healthcare costs by preventing unnecessary procedures. Secondly, it helps to prevent adverse reactions and interactions between medications, promoting patient safety. Lastly, prior authorization helps to streamline the billing process, reducing the likelihood of denied claims and delayed payments.
Understanding the Blue Advantage Prior Authorization Form

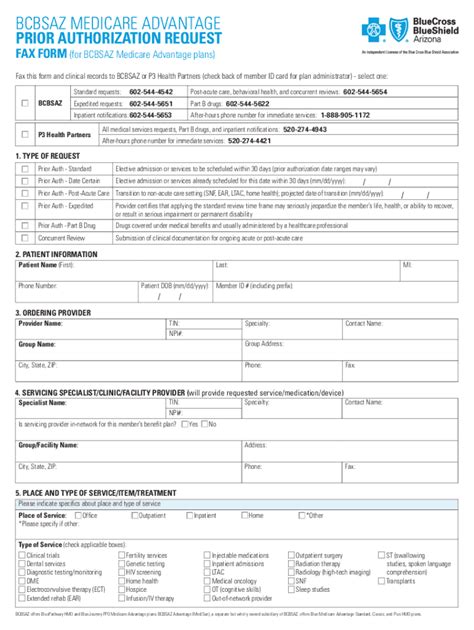
The Blue Advantage prior authorization form is a document that healthcare providers must complete and submit to Blue Cross Blue Shield (BCBS) to obtain approval for a patient's treatment or medication. The form requires detailed information about the patient, the treatment or medication being requested, and the medical justification for the request. The form typically includes the following sections:
- Patient demographics
- Treatment or medication information
- Medical justification
- Supporting documentation
Key Components of the Blue Advantage Prior Authorization Form
To ensure a smooth prior authorization process, it is essential to understand the key components of the Blue Advantage prior authorization form. The following are some of the critical sections of the form:
- Patient demographics: This section requires the patient's name, date of birth, policy number, and other identifying information.
- Treatment or medication information: This section requires details about the treatment or medication being requested, including the name, dosage, and frequency.
- Medical justification: This section requires a detailed explanation of the medical justification for the requested treatment or medication. This may include information about the patient's diagnosis, medical history, and any previous treatments.
- Supporting documentation: This section requires supporting documentation, such as medical records, test results, and physician statements, to justify the requested treatment or medication.
Mastery of the Blue Advantage Prior Authorization Process

Mastering the Blue Advantage prior authorization process requires a deep understanding of the form and the necessary documentation. The following are some tips to help healthcare providers master the process:
- Understand the requirements: Take the time to review the Blue Advantage prior authorization form and understand the requirements for each section.
- Gather supporting documentation: Gather all necessary supporting documentation, including medical records, test results, and physician statements, to justify the requested treatment or medication.
- Complete the form accurately: Complete the form accurately and thoroughly, ensuring that all required information is included.
- Submit the form timely: Submit the form in a timely manner, allowing sufficient time for BCBS to review and process the request.
Tips for Successful Prior Authorization
To ensure successful prior authorization, healthcare providers should follow these tips:
- Verify patient eligibility: Verify the patient's eligibility and benefits before submitting the prior authorization request.
- Use the correct form: Use the correct Blue Advantage prior authorization form for the specific treatment or medication being requested.
- Provide detailed information: Provide detailed information about the patient's condition and the requested treatment or medication.
- Follow up: Follow up with BCBS to ensure that the request is processed in a timely manner.
Common Challenges and Solutions

Despite the importance of prior authorization, healthcare providers often face challenges during the process. The following are some common challenges and solutions:
- Incomplete or inaccurate information: Ensure that all required information is included and accurate to avoid delays or denials.
- Insufficient supporting documentation: Gather all necessary supporting documentation to justify the requested treatment or medication.
- Delays in processing: Follow up with BCBS to ensure that the request is processed in a timely manner.
Best Practices for Streamlining the Prior Authorization Process
To streamline the prior authorization process, healthcare providers should follow these best practices:
- Implement a prior authorization workflow: Implement a prior authorization workflow to ensure that all necessary steps are taken and documentation is gathered.
- Use electronic prior authorization: Use electronic prior authorization to reduce paperwork and increase efficiency.
- Designate a prior authorization coordinator: Designate a prior authorization coordinator to manage the process and ensure that all necessary steps are taken.
What is the purpose of prior authorization?
+Prior authorization is a step in the healthcare process that ensures patients receive the necessary treatment while also controlling healthcare costs.
What is the Blue Advantage prior authorization form?
+The Blue Advantage prior authorization form is a document that healthcare providers must complete and submit to Blue Cross Blue Shield (BCBS) to obtain approval for a patient's treatment or medication.
How can healthcare providers master the Blue Advantage prior authorization process?
+Healthcare providers can master the Blue Advantage prior authorization process by understanding the form and necessary documentation, gathering supporting documentation, completing the form accurately, and submitting the form in a timely manner.
By mastering the Blue Advantage prior authorization form and process, healthcare providers can ensure that patients receive the necessary treatment while also controlling healthcare costs. Remember to verify patient eligibility, use the correct form, provide detailed information, and follow up with BCBS to ensure a smooth prior authorization process.