The Benecard prior authorization form - a crucial step in ensuring that patients receive the necessary medications while also controlling healthcare costs. As a healthcare provider, navigating the prior authorization process can be daunting, but fear not! In this article, we will break down the Benecard prior authorization form into 5 easy steps, making it easier for you to get the necessary approvals for your patients.
The Importance of Prior Authorization
Prior authorization is a process used by health insurance companies to determine whether a particular medication or treatment is medically necessary and covered under the patient's insurance plan. While it may seem like an extra hoop to jump through, prior authorization is essential in controlling healthcare costs and ensuring that patients receive the most effective treatments. Benecard, a leading pharmacy benefit manager, requires prior authorization for certain medications to ensure that patients receive the best possible care while also managing costs.
Step 1: Determine If Prior Authorization Is Required
Before starting the prior authorization process, you need to determine if it's required for the specific medication or treatment you're prescribing. Benecard provides a list of medications that require prior authorization on their website. You can also contact Benecard's customer service to confirm whether prior authorization is needed.

Step 2: Gather Necessary Information
Once you've determined that prior authorization is required, it's time to gather the necessary information. You'll need to collect the patient's medical records, including their diagnosis, medical history, and any relevant test results. You'll also need to provide information about the medication or treatment you're prescribing, including the dosage and duration of treatment.
Step 3: Complete the Benecard Prior Authorization Form
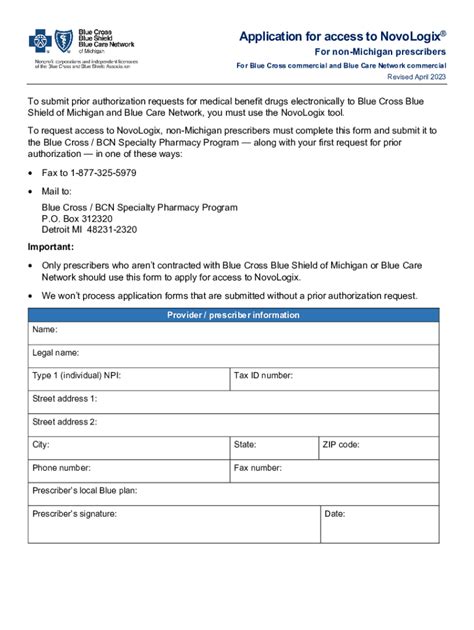
Now it's time to complete the Benecard prior authorization form. The form can be downloaded from Benecard's website or requested by contacting their customer service. The form will ask for the patient's information, the medication or treatment being prescribed, and the medical justification for the request. Be sure to complete the form accurately and thoroughly, as incomplete or inaccurate information can delay the prior authorization process.

Step 4: Submit the Prior Authorization Request
Once the form is complete, it's time to submit the prior authorization request to Benecard. You can submit the request online, by phone, or by fax. Be sure to follow Benecard's submission guidelines carefully to avoid any delays in the process.
Step 5: Follow Up on the Prior Authorization Request
After submitting the prior authorization request, it's essential to follow up with Benecard to ensure that the request is being processed. You can check the status of the request online or by contacting Benecard's customer service. If the request is approved, Benecard will notify you and the patient's pharmacy. If the request is denied, you can appeal the decision by providing additional information or clarification.

Benefits of Benecard Prior Authorization Form
While the prior authorization process may seem like an extra step, it has several benefits for patients and healthcare providers. By ensuring that medications and treatments are medically necessary, prior authorization can help control healthcare costs and reduce the risk of adverse reactions. Additionally, prior authorization can help ensure that patients receive the most effective treatments for their conditions.
Common Mistakes to Avoid
When completing the Benecard prior authorization form, there are several common mistakes to avoid. These include:
- Incomplete or inaccurate information
- Failure to provide medical justification for the request
- Not following Benecard's submission guidelines
- Not following up on the prior authorization request
By avoiding these common mistakes, you can ensure that the prior authorization process goes smoothly and that your patients receive the necessary medications and treatments.
Conclusion
In conclusion, the Benecard prior authorization form may seem like a daunting task, but by following these 5 easy steps, you can ensure that your patients receive the necessary medications and treatments. Remember to determine if prior authorization is required, gather necessary information, complete the form accurately, submit the request, and follow up on the request. By following these steps and avoiding common mistakes, you can streamline the prior authorization process and provide the best possible care for your patients.
What is the purpose of prior authorization?
+Prior authorization is used by health insurance companies to determine whether a particular medication or treatment is medically necessary and covered under the patient's insurance plan.
How do I know if prior authorization is required for a medication?
+You can check Benecard's website for a list of medications that require prior authorization or contact their customer service to confirm.
What information do I need to provide for the prior authorization request?
+You'll need to provide the patient's medical records, including their diagnosis, medical history, and any relevant test results, as well as information about the medication or treatment being prescribed.