When dealing with denied claims or coverage issues, understanding the appeal process is crucial for resolving disputes with your health insurance provider. For those insured by BlueCross BlueShield of Tennessee (BCBS TN), one of the steps in this process involves submitting a reconsideration form. This article will guide you through the 5 steps to complete a BCBS TN reconsideration form effectively, helping you navigate the often-complex world of health insurance appeals.
Understanding the Reconsideration Process
Before diving into the steps, it's essential to grasp what the reconsideration process entails. A reconsideration is essentially a request to review a previously denied claim or decision, hoping to reverse or modify it in your favor. This process is usually initiated after an initial denial, and it's a precursor to further appeal levels if the decision isn't favorable. It's a critical step in advocating for your healthcare coverage rights.

Step 1: Review Your Denial Letter
The journey begins with thoroughly reviewing the denial letter you received from BCBS TN. This letter should outline the reasons for the denial, along with information on how to appeal the decision. It's crucial to understand the specific grounds for denial, as this will guide the content of your reconsideration request. Look for details such as the claim number, the date of the denial, and any relevant policy numbers.
Step 2: Gather Supporting Documentation
Your reconsideration form will need to be supported by additional documentation that strengthens your case. This could include:
- Medical Records: Any new medical information or records that were not previously considered can be crucial.
- Clinical Information: Supporting documents from healthcare providers can clarify the medical necessity of the denied service.
- Policy Details: Highlight any policy terms or conditions that support your case.
Make sure all documentation is organized, and include a cover letter or introduction explaining the purpose of each document.

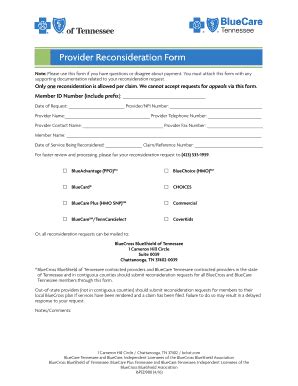
Step 3: Complete the Reconsideration Form
BCBS TN will typically provide a specific form for reconsideration requests. This form will ask for:
- Personal and Policy Information: Your name, policy number, claim number, and contact details.
- Details of the Denied Claim: The date of the denied claim and a description of the service or treatment denied.
- Reasons for Reconsideration: Here, you will explain why you believe the denial was incorrect and provide a brief overview of your supporting documentation.
Ensure you fill out the form accurately and completely. Missing information can delay the process.
Step 4: Submit Your Request
Once your form and supporting documents are ready, submit them according to the instructions provided by BCBS TN. This might involve mailing the documents to a specific address or uploading them through an online portal. Keep a record of your submission, including the date and any tracking numbers, for future reference.

Step 5: Follow Up
After submitting your reconsideration request, it's essential to follow up with BCBS TN. This ensures that your request has been received and is being processed. You can do this via phone or by checking the status online, if available. Keep track of any communication, including dates, times, and the names of representatives you speak with.

Navigating the Reconsideration Process with Ease
While the reconsideration process can seem daunting, breaking it down into these manageable steps can make the task less overwhelming. Remember, the key to a successful reconsideration is thorough preparation and clear communication. Don't hesitate to seek help if you're unsure about any part of the process.
By following these steps and staying committed to your appeal, you're taking proactive steps towards resolving your insurance dispute. Keep in mind that persistence and patience are your allies in navigating the complex healthcare system.
We hope this guide has been informative and helpful. If you have any further questions or need additional guidance, please don't hesitate to reach out or leave a comment below.
What is a reconsideration in the context of health insurance?
+A reconsideration is a request to review a previously denied claim or decision, with the hope of reversing or modifying it in your favor.
How long does the reconsideration process typically take?
+The duration of the reconsideration process can vary, but it usually takes several weeks to a few months. It's essential to follow up with your insurance provider for updates.
Can I seek help from a professional if I'm unsure about the reconsideration process?
+Yes, if you're unsure about any part of the reconsideration process, you can seek help from a patient advocate or a healthcare attorney who specializes in insurance disputes.