In the world of healthcare, navigating the complex landscape of insurance claims and pre-authorizations can be a daunting task for medical professionals and patients alike. One essential tool in this process is the BCBS of TX Predetermination Form, used by Blue Cross Blue Shield of Texas to assess the medical necessity of proposed treatments. Understanding the intricacies of this form is crucial for ensuring that patients receive the care they need while minimizing the risk of claim denials. In this article, we will guide you through the 5 steps to achieving success with the BCBS of TX Predetermination Form.
Step 1: Understanding the Purpose and Requirements of the BCBS of TX Predetermination Form

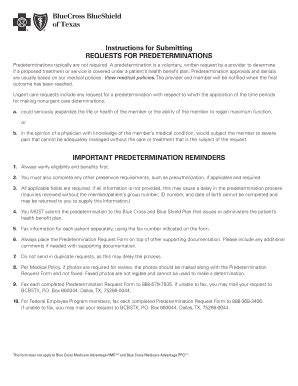
The BCBS of TX Predetermination Form is designed to evaluate whether a proposed treatment or service is medically necessary and aligns with the patient's policy coverage. To ensure a smooth process, it's essential to understand the specific requirements of the form, including the necessary documentation, coding, and medical information. Providers must also be aware of the specific policies and procedures outlined by BCBS of TX, as these can vary depending on the patient's plan.
Key Elements to Include:
- Patient's medical history and current condition
- Proposed treatment or service, including CPT/HCPCS codes
- Supporting documentation, such as medical records and test results
- Statement of medical necessity
- Plan details and policy numbers
Step 2: Gathering and Preparing Required Documentation

The next step in achieving success with the BCBS of TX Predetermination Form is to gather and prepare the required documentation. This includes the patient's medical history, current condition, and any relevant test results or medical records. Providers must ensure that all documentation is accurate, up-to-date, and complete, as any missing or incomplete information can lead to delays or denials.
Best Practices for Documenting Medical Necessity:
- Use clear and concise language
- Include relevant medical terminology and codes
- Provide detailed explanations of proposed treatments and services
- Attach supporting documentation, such as lab results and imaging studies
Step 3: Completing the BCBS of TX Predetermination Form Accurately

With the necessary documentation in hand, the next step is to complete the BCBS of TX Predetermination Form accurately. Providers must ensure that all sections are filled out correctly, including patient information, proposed treatments, and medical necessity statements. It's essential to follow the instructions carefully and avoid any errors or omissions that could lead to delays or denials.
Common Mistakes to Avoid:
- Incomplete or missing information
- Incorrect coding or billing information
- Failure to include supporting documentation
- Inconsistent or unclear medical necessity statements
Step 4: Submitting the BCBS of TX Predetermination Form and Tracking Status

Once the BCBS of TX Predetermination Form is complete, the next step is to submit it to BCBS of TX for review. Providers can submit the form via fax, email, or online portal, depending on the preferred method. It's essential to track the status of the submission and follow up with BCBS of TX as needed to ensure a timely decision.
Tracking Status and Following Up:
- Verify receipt of the submission
- Track the status of the review process
- Follow up with BCBS of TX if necessary
- Respond to any additional requests for information
Step 5: Responding to BCBS of TX Predetermination Form Decisions

The final step in achieving success with the BCBS of TX Predetermination Form is to respond to the decision made by BCBS of TX. Providers must review the decision carefully and respond accordingly, whether it's to appeal a denial or proceed with the approved treatment. It's essential to understand the appeals process and the necessary steps to take if a denial is received.
Understanding the Appeals Process:
- Review the decision and reason for denial
- Gather additional information or documentation as needed
- Submit an appeal within the designated timeframe
- Follow up with BCBS of TX to ensure receipt and review of the appeal
What is the purpose of the BCBS of TX Predetermination Form?
+The BCBS of TX Predetermination Form is used to evaluate whether a proposed treatment or service is medically necessary and aligns with the patient's policy coverage.
What documentation is required to complete the BCBS of TX Predetermination Form?
+The required documentation includes the patient's medical history, current condition, and any relevant test results or medical records, as well as a statement of medical necessity and plan details.
How do I track the status of my BCBS of TX Predetermination Form submission?
+Providers can track the status of their submission by verifying receipt with BCBS of TX, tracking the review process, and following up as needed.
By following these 5 steps and understanding the intricacies of the BCBS of TX Predetermination Form, providers can ensure a smooth and successful process for their patients. Remember to stay informed, gather necessary documentation, complete the form accurately, track status, and respond to decisions accordingly.