The predetermination process is an essential step in ensuring that medical treatments and procedures are covered by insurance providers. For individuals with Blue Cross Blue Shield of Illinois (BCBS IL) insurance, understanding the predetermination form and process is crucial to avoid unexpected medical bills. In this article, we will provide a step-by-step guide on how to complete the BCBS IL predetermination form and what to expect during the process.
Why is Predetermination Important?

Predetermination is a process that allows healthcare providers to verify the medical necessity of a treatment or procedure before it is performed. This process helps ensure that the treatment is covered by the insurance provider, reducing the risk of unexpected medical bills. By obtaining predetermination, patients can:
- Confirm coverage for a specific treatment or procedure
- Understand the estimated costs and out-of-pocket expenses
- Avoid surprise medical bills
- Make informed decisions about their care
What is the BCBS IL Predetermination Form?

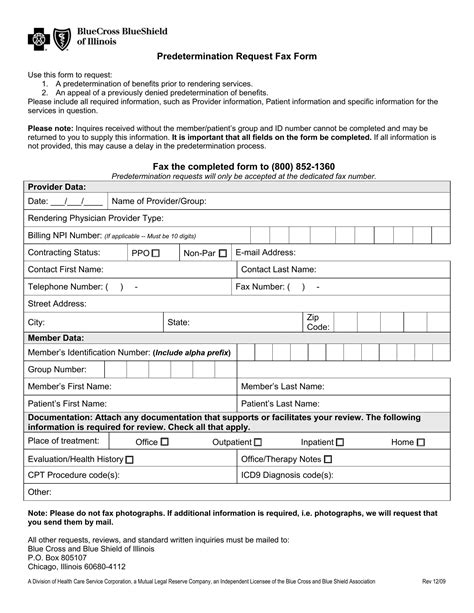
The BCBS IL predetermination form is a document that healthcare providers complete to request predetermination for a specific treatment or procedure. The form requires detailed information about the patient, the treatment or procedure, and the diagnosis. The form typically includes the following sections:
- Patient information
- Treatment or procedure information
- Diagnosis and medical necessity
- Estimated costs and billing information
Step 1: Gather Required Information
Before completing the predetermination form, healthcare providers must gather the required information, including:
- Patient demographics and insurance information
- Treatment or procedure details, including CPT codes and descriptions
- Diagnosis and medical necessity information, including ICD-10 codes
- Estimated costs and billing information
Step 2: Complete the Predetermination Form
Once the required information is gathered, the healthcare provider can complete the predetermination form. The form should be completed accurately and thoroughly, as incomplete or inaccurate information may delay or deny the predetermination request.
How to Submit the Predetermination Form

The completed predetermination form can be submitted to BCBS IL through various channels, including:
- Fax: Healthcare providers can fax the completed form to the designated BCBS IL fax number.
- Online Portal: BCBS IL offers an online portal for healthcare providers to submit predetermination requests electronically.
- Mail: Healthcare providers can mail the completed form to the designated BCBS IL address.
Step 3: Wait for Predetermination Decision
After submitting the predetermination form, the healthcare provider will receive a decision from BCBS IL within a specified timeframe, typically 3-5 business days. The decision will indicate whether the treatment or procedure is covered, partially covered, or not covered.
What to Expect During the Predetermination Process

During the predetermination process, healthcare providers and patients can expect:
- A thorough review of the predetermination request
- Verification of coverage and medical necessity
- An estimate of costs and out-of-pocket expenses
- A decision on coverage, which may include conditions or limitations
Tips for Healthcare Providers
To ensure a smooth predetermination process, healthcare providers should:
- Complete the predetermination form accurately and thoroughly
- Submit the form well in advance of the treatment or procedure
- Follow up with BCBS IL to ensure timely processing
- Communicate with patients about the predetermination decision and estimated costs
Conclusion: Taking Control of Your Healthcare

By understanding the BCBS IL predetermination form and process, patients and healthcare providers can take control of their healthcare and avoid unexpected medical bills. By following the steps outlined in this guide, individuals can ensure that their medical treatments and procedures are covered by their insurance provider.
We encourage you to share your experiences and tips for navigating the predetermination process in the comments below. Additionally, if you have any questions or concerns about the BCBS IL predetermination form or process, please don't hesitate to ask.
What is predetermination, and why is it important?
+Predetermination is a process that allows healthcare providers to verify the medical necessity of a treatment or procedure before it is performed. This process helps ensure that the treatment is covered by the insurance provider, reducing the risk of unexpected medical bills.
How long does the predetermination process take?
+The predetermination process typically takes 3-5 business days, but may vary depending on the complexity of the request and the workload of the insurance provider.
Can I appeal a denied predetermination request?
+Yes, patients and healthcare providers can appeal a denied predetermination request. The appeal process typically involves submitting additional information or documentation to support the medical necessity of the treatment or procedure.