The healthcare landscape can be complex and overwhelming, especially when it comes to navigating the intricacies of insurance coverage. For individuals and healthcare providers in Illinois, understanding the BCBS (Blue Cross Blue Shield) predetermination process is crucial for ensuring seamless and cost-effective care. In this article, we will delve into the world of BCBS Illinois predetermination forms, exploring their significance, benefits, and step-by-step instructions for submission.
Understanding BCBS Illinois Predetermination

Predetermination, also known as prior authorization or pre-certification, is a process used by health insurance providers like BCBS Illinois to evaluate the medical necessity of a proposed treatment or service. This assessment is typically required for non-emergency procedures, such as surgeries, hospital stays, or high-cost diagnostic tests. By submitting a predetermination form, healthcare providers can obtain a preliminary determination of coverage before rendering services, helping to prevent unexpected costs and financial burdens on patients.
Why is BCBS Illinois Predetermination Important?
- Financial Protection: Predetermination helps protect patients from unexpected medical bills by verifying coverage before services are rendered.
- Streamlined Care: By obtaining prior authorization, healthcare providers can ensure that necessary services are covered, reducing the risk of delayed or denied treatments.
- Cost Savings: Predetermination can help prevent unnecessary procedures or services, leading to cost savings for patients, providers, and insurers.
The BCBS Illinois Predetermination Form: A Step-by-Step Guide

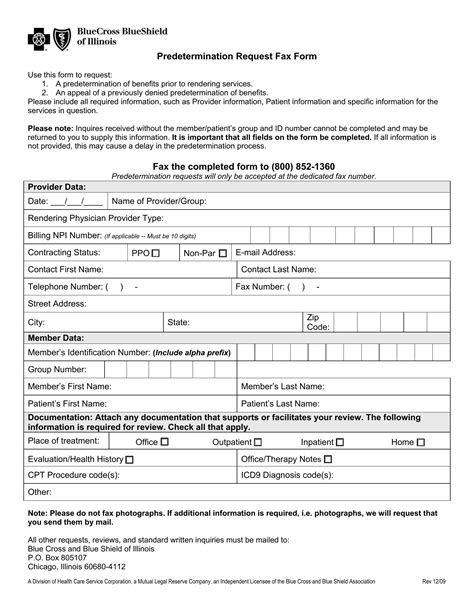
The BCBS Illinois predetermination form is typically completed by the healthcare provider or their staff. Here's a step-by-step guide to help you navigate the process:
Step 1: Gather Required Information
- Patient's demographic and insurance information
- Proposed treatment or service details (including dates, locations, and CPT codes)
- Clinical information and supporting documentation (e.g., medical records, test results)
Step 2: Complete the Predetermination Form
- Download and complete the BCBS Illinois predetermination form (available on the BCBS Illinois website or through your provider portal)
- Ensure all required fields are completed accurately and thoroughly
Step 3: Submit the Form
- Fax the completed form to BCBS Illinois at the designated fax number
- Alternatively, submit the form electronically through the BCBS Illinois provider portal
Step 4: Receive Determination
- BCBS Illinois will review the submission and provide a determination of coverage
- The determination will be sent to the healthcare provider and patient (if requested)
Tips for a Smooth Predetermination Process
- Submit complete and accurate information to avoid delays or denials.
- Use the correct form and follow the submission guidelines.
- Allow sufficient time for review and determination (typically 3-5 business days).
- Keep patients informed about the predetermination process and any updates.
Frequently Asked Questions
What is the purpose of the BCBS Illinois predetermination form?
+The BCBS Illinois predetermination form is used to evaluate the medical necessity of a proposed treatment or service, ensuring coverage and preventing unexpected costs.
Who completes the BCBS Illinois predetermination form?
+The healthcare provider or their staff typically completes the predetermination form.
How long does the predetermination process take?
+The predetermination process typically takes 3-5 business days, but may vary depending on the complexity of the request.
By understanding the BCBS Illinois predetermination process and following the step-by-step guide, healthcare providers can ensure a smoother and more efficient experience for their patients. Remember to submit complete and accurate information, use the correct form, and allow sufficient time for review and determination. If you have any further questions or concerns, don't hesitate to reach out to BCBS Illinois or your provider portal for assistance.