The prior authorization process can be a complex and time-consuming step in receiving medical treatment. For members of the Blue Cross Blue Shield Federal Employee Program (BCBS FEP), understanding the prior authorization form and process is crucial to ensure that necessary treatments are approved and covered by the insurance plan. In this article, we will delve into the world of BCBS FEP prior authorization forms, providing a comprehensive guide on how to navigate the process, common challenges, and best practices to ensure a smooth experience.
Understanding Prior Authorization
Prior authorization is a requirement by health insurance companies, including BCBS FEP, to review and approve certain medical treatments, services, or medications before they are administered. This process aims to ensure that members receive necessary and cost-effective care while preventing unnecessary or experimental treatments. Prior authorization is typically required for non-emergency services, such as surgical procedures, specialty medications, or high-cost diagnostic tests.

BCBS FEP Prior Authorization Form
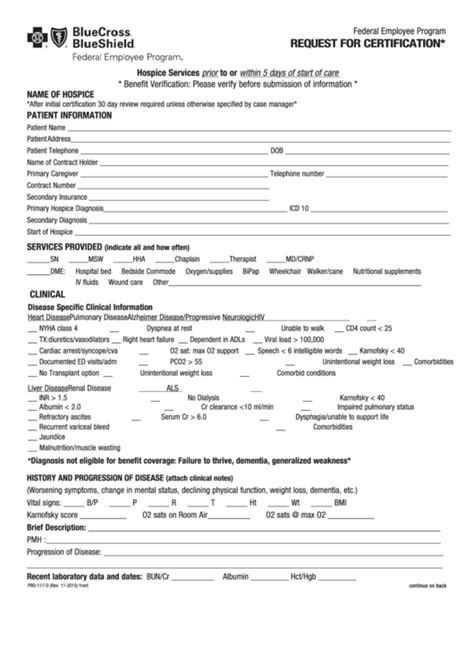
The BCBS FEP prior authorization form is a critical document that healthcare providers must submit to the insurance company to request approval for a specific medical treatment or service. The form requires detailed information about the patient's condition, the proposed treatment, and the provider's justification for the treatment. The form typically includes the following sections:
- Patient information
- Treatment or service details
- Provider information
- Justification for treatment
- Supporting documentation (e.g., medical records, test results)
Steps to Complete the BCBS FEP Prior Authorization Form
To ensure a successful prior authorization process, healthcare providers should follow these steps:
- Verify coverage: Confirm that the patient is a BCBS FEP member and that the proposed treatment is covered under their plan.
- Gather necessary documentation: Collect relevant medical records, test results, and other supporting documentation to justify the treatment.
- Complete the prior authorization form: Fill out the form accurately and thoroughly, ensuring that all required sections are completed.
- Submit the form: Send the completed form to BCBS FEP via fax, email, or online portal.
- Follow up: If necessary, follow up with BCBS FEP to confirm receipt of the form and to inquire about the status of the prior authorization request.
Common Challenges and Solutions
Despite the importance of prior authorization, the process can be complex and time-consuming, leading to delays in treatment. Some common challenges and solutions include:
- Incomplete or inaccurate forms: Ensure that the form is completed thoroughly and accurately to avoid delays or denials.
- Lack of supporting documentation: Gather all necessary documentation to support the prior authorization request.
- Insufficient justification: Provide clear and concise justification for the proposed treatment.
- Communication breakdowns: Establish open communication with BCBS FEP and the patient to ensure that all parties are informed about the prior authorization status.

Best Practices for Healthcare Providers
To ensure a smooth prior authorization process, healthcare providers should follow these best practices:
- Verify coverage and prior authorization requirements: Confirm that the patient is a BCBS FEP member and that prior authorization is required for the proposed treatment.
- Use the correct prior authorization form: Ensure that the correct form is used for the specific treatment or service.
- Submit complete and accurate forms: Complete the form thoroughly and accurately to avoid delays or denials.
- Follow up: Follow up with BCBS FEP to confirm receipt of the form and to inquire about the status of the prior authorization request.
Conclusion
The BCBS FEP prior authorization form is a critical component of the prior authorization process, ensuring that members receive necessary and cost-effective care. By understanding the prior authorization process, completing the form accurately, and following best practices, healthcare providers can help ensure a smooth experience for their patients. If you have any questions or concerns about the prior authorization process, we encourage you to reach out to BCBS FEP or your healthcare provider.

Take Action
We invite you to share your experiences with the prior authorization process in the comments below. Have you encountered any challenges or successes with the BCBS FEP prior authorization form? Your feedback can help others navigate the process more effectively.
What is prior authorization?
+Prior authorization is a requirement by health insurance companies to review and approve certain medical treatments, services, or medications before they are administered.
Why is prior authorization required?
+Prior authorization is required to ensure that members receive necessary and cost-effective care while preventing unnecessary or experimental treatments.
How do I complete the BCBS FEP prior authorization form?
+Complete the form accurately and thoroughly, ensuring that all required sections are completed. Gather necessary documentation, such as medical records and test results, to support the prior authorization request.