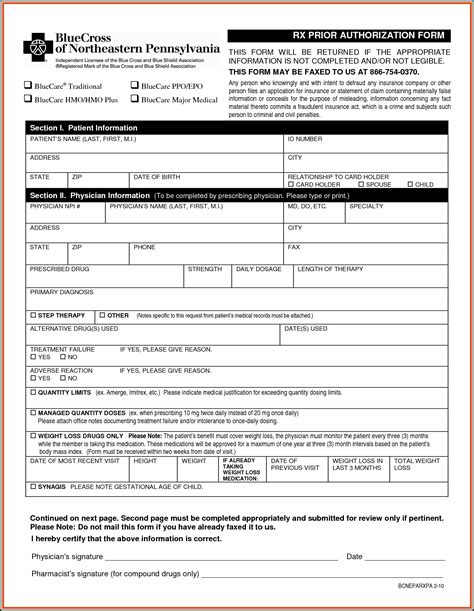
The Blue Cross Blue Shield Federal Employee Program (BCBS FEP) prior authorization form is an essential document that healthcare providers must submit to obtain approval for certain medical procedures and treatments. However, the traditional submission process can be complex, time-consuming, and prone to errors. In this article, we will explore the BCBS FEP prior auth form and discuss how to simplify the submission process.
Understanding the Importance of Prior Authorization
Prior authorization is a critical step in ensuring that patients receive medically necessary treatments while also controlling healthcare costs. By reviewing and approving treatment plans before they are administered, insurance providers can verify that the treatments are necessary, safe, and cost-effective. For healthcare providers, prior authorization can help prevent denied claims, reduce administrative burdens, and improve patient outcomes.
Challenges with Traditional Prior Authorization Submissions
The traditional prior authorization submission process can be cumbersome and inefficient. Healthcare providers must manually complete and submit the BCBS FEP prior auth form, which can lead to errors, delays, and frustration. Some of the common challenges associated with traditional submissions include:
- Incomplete or inaccurate forms
- Delays in processing and approval
- Lack of transparency and communication
- Increased administrative burdens
Streamlining the Prior Authorization Process
Fortunately, there are ways to simplify the prior authorization submission process. Here are some strategies that healthcare providers can use to streamline their submissions:
Electronic Submission
One of the most effective ways to simplify the prior authorization process is to use electronic submission methods. Many insurance providers, including BCBS FEP, offer online portals or electronic health record (EHR) systems that allow healthcare providers to submit prior authorization requests electronically. This approach can reduce errors, increase efficiency, and speed up the approval process.

Standardized Forms
Using standardized prior authorization forms can also help simplify the submission process. Standardized forms can reduce errors, increase efficiency, and ensure that all required information is included. Healthcare providers can use templates or software to generate standardized forms, which can be easily submitted electronically.
Automated Workflows
Automated workflows can also help streamline the prior authorization process. Automated workflows can help healthcare providers track and manage prior authorization requests, receive notifications, and receive approval or denial notifications.
Communication and Transparency
Effective communication and transparency are critical to a successful prior authorization process. Healthcare providers should communicate clearly with patients, insurance providers, and other stakeholders to ensure that everyone is informed and up-to-date on the status of prior authorization requests.
Best Practices for BCBS FEP Prior Auth Form Submissions
To ensure a smooth and efficient prior authorization submission process, healthcare providers should follow these best practices:
Verify Patient Eligibility
Before submitting a prior authorization request, healthcare providers should verify patient eligibility and benefits.
Use Standardized Forms
Healthcare providers should use standardized prior authorization forms to reduce errors and increase efficiency.
Submit Requests Electronically
Whenever possible, healthcare providers should submit prior authorization requests electronically to reduce errors and increase efficiency.
Track and Follow Up
Healthcare providers should track and follow up on prior authorization requests to ensure that they are processed in a timely manner.

Common FAQs about BCBS FEP Prior Auth Form Submissions
Here are some frequently asked questions about BCBS FEP prior auth form submissions:
What is the BCBS FEP prior auth form?
+The BCBS FEP prior auth form is a document that healthcare providers must submit to obtain approval for certain medical procedures and treatments.
How can I simplify the prior authorization submission process?
+Healthcare providers can simplify the prior authorization submission process by using electronic submission methods, standardized forms, automated workflows, and effective communication and transparency.
What are some common challenges associated with traditional prior authorization submissions?
+Common challenges associated with traditional prior authorization submissions include incomplete or inaccurate forms, delays in processing and approval, lack of transparency and communication, and increased administrative burdens.
Conclusion
The BCBS FEP prior auth form is an essential document that healthcare providers must submit to obtain approval for certain medical procedures and treatments. However, the traditional submission process can be complex, time-consuming, and prone to errors. By using electronic submission methods, standardized forms, automated workflows, and effective communication and transparency, healthcare providers can simplify the prior authorization submission process and improve patient outcomes.