In the state of Arkansas, Medicaid provides essential healthcare coverage to low-income individuals and families. To ensure the provision of necessary medical services while controlling costs, Arkansas Medicaid has implemented a prior authorization (PA) process. This process requires healthcare providers to obtain approval from Medicaid before administering certain medical treatments or services. In this article, we will delve into the Arkansas Medicaid prior authorization form guide, explaining the purpose, benefits, and steps involved in the process.

Understanding Prior Authorization
Prior authorization is a critical component of the Arkansas Medicaid program, enabling the state to manage healthcare costs while ensuring that beneficiaries receive medically necessary services. The PA process involves a review of a patient's medical condition, treatment plan, and the requested service or medication to determine whether it is medically necessary and meets Medicaid's coverage criteria.
Benefits of Prior Authorization
The prior authorization process offers several benefits, including:
- Ensuring that patients receive medically necessary services
- Reducing healthcare costs by avoiding unnecessary treatments
- Improving patient outcomes by promoting evidence-based care
- Enhancing communication between healthcare providers and Medicaid
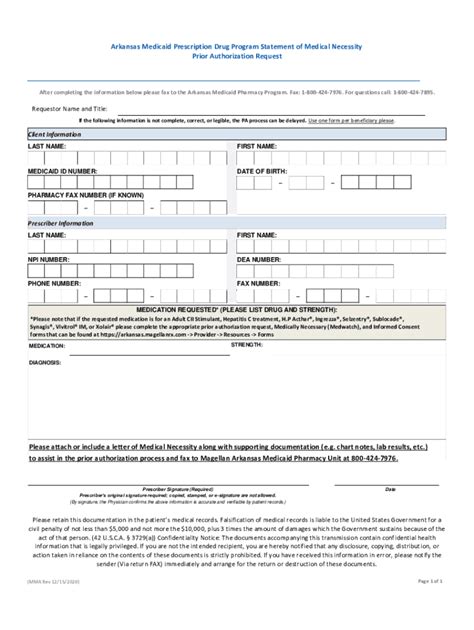
Arkansas Medicaid Prior Authorization Form
To initiate the prior authorization process, healthcare providers must submit a prior authorization request form to Arkansas Medicaid. The form requires the following information:
- Patient demographics and Medicaid ID number
- Diagnosis and treatment plan
- Requested service or medication
- Clinical rationale for the requested service or medication
- Supporting documentation, such as medical records and test results
Step-by-Step Guide to the Prior Authorization Process
- Determine the need for prior authorization: Healthcare providers must check the Arkansas Medicaid fee schedule and coverage policies to determine if prior authorization is required for the requested service or medication.
- Gather required documentation: Providers must collect the necessary documentation, including medical records, test results, and treatment plans.
- Complete the prior authorization request form: Providers must submit a completed prior authorization request form to Arkansas Medicaid.
- Submit the request: Providers can submit the request via fax, mail, or online portal.
- Review and approval: Arkansas Medicaid will review the request and approve or deny it based on medical necessity and coverage criteria.
- Notification: Providers will receive notification of the approval or denial decision.
Common Prior Authorization Forms
Arkansas Medicaid uses several prior authorization forms, including:
- PA-1: Prior Authorization Request Form for Medical Services
- PA-2: Prior Authorization Request Form for Pharmacy Services
- PA-3: Prior Authorization Request Form for Durable Medical Equipment (DME)
Tips for Submitting a Successful Prior Authorization Request
- Ensure that the request form is complete and accurate
- Provide clear and concise clinical rationale for the requested service or medication
- Submit supporting documentation, such as medical records and test results
- Follow up with Arkansas Medicaid to ensure timely processing of the request
Challenges and Solutions
Common challenges encountered during the prior authorization process include:
- Delays in processing: Ensure timely submission of requests and follow up with Arkansas Medicaid to avoid delays.
- Denials: Provide clear and concise clinical rationale and submit supporting documentation to reduce the likelihood of denials.
- Complexity: Use online resources and Medicaid's provider manual to navigate the prior authorization process.
Conclusion and Next Steps
In conclusion, the Arkansas Medicaid prior authorization form guide is an essential resource for healthcare providers seeking to navigate the prior authorization process. By understanding the purpose, benefits, and steps involved in the process, providers can ensure that their patients receive medically necessary services while minimizing delays and denials. We encourage providers to share their experiences and tips for submitting successful prior authorization requests in the comments section below.
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from Medicaid before administering certain medical treatments or services.
How do I submit a prior authorization request?
+Providers can submit prior authorization requests via fax, mail, or online portal.
What are the common prior authorization forms used by Arkansas Medicaid?
+Arkansas Medicaid uses several prior authorization forms, including PA-1, PA-2, and PA-3.