Prior authorization (prior auth) is a crucial process in healthcare that ensures patients receive necessary medical treatments while preventing unnecessary costs and potential harm. In Arkansas, Blue Cross Blue Shield (BCBS) is one of the leading health insurance providers that requires prior auth for certain medical procedures and services. In this article, we will delve into the Arkansas Blue Cross Blue Shield prior auth form guide, providing an in-depth understanding of the process, benefits, and requirements.

What is Prior Authorization (Prior Auth)?
Prior authorization is a healthcare process where a patient's insurance provider reviews and approves a treatment or service before it is rendered. This process ensures that the proposed treatment is medically necessary, safe, and meets the insurance provider's coverage criteria. Prior auth is usually required for high-cost or specialized treatments, such as surgeries, hospital stays, or expensive medications.
Why is Prior Auth Important?
Prior auth is essential for several reasons:
- Patient Safety: Prior auth helps ensure that patients receive safe and effective treatments. By reviewing the proposed treatment, insurance providers can identify potential risks or contraindications.
- Cost Savings: Prior auth helps reduce unnecessary healthcare costs by preventing treatments that are not medically necessary or are unlikely to be effective.
- Quality of Care: Prior auth promotes high-quality care by ensuring that patients receive evidence-based treatments that meet clinical guidelines.
Arkansas Blue Cross Blue Shield Prior Auth Requirements
Arkansas BCBS requires prior auth for various medical services and treatments. The following are some examples of services that may require prior auth:
- Inpatient Hospital Services: Hospital stays, surgeries, and other inpatient services may require prior auth.
- Outpatient Services: Certain outpatient services, such as physical therapy, speech therapy, or occupational therapy, may require prior auth.
- Pharmacy Services: Some medications, especially high-cost or specialty medications, may require prior auth.
- Durable Medical Equipment (DME): DME, such as wheelchairs, oxygen tanks, or diabetic supplies, may require prior auth.

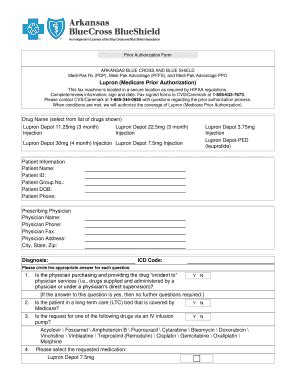
Arkansas Blue Cross Blue Shield Prior Auth Form
The Arkansas BCBS prior auth form is a standardized document used to request prior auth for medical services or treatments. The form typically includes the following information:
- Patient Information: Patient name, date of birth, and insurance ID number.
- Provider Information: Provider name, contact information, and NPI number.
- Service or Treatment Information: Description of the service or treatment being requested, including CPT codes and diagnosis codes.
- Clinical Information: Relevant clinical information, such as medical history and lab results.
How to Submit a Prior Auth Request
To submit a prior auth request to Arkansas BCBS, providers can follow these steps:
- Online Portal: Submit the request through the Arkansas BCBS online portal, which is available 24/7.
- Phone: Call the Arkansas BCBS prior auth hotline, which is available Monday through Friday, 8 am to 5 pm.
- Fax: Fax the completed prior auth form to the Arkansas BCBS fax number.

Arkansas Blue Cross Blue Shield Prior Auth Timeline
The prior auth timeline varies depending on the type of service or treatment being requested. The following are some general guidelines:
- Urgent Requests: Urgent requests, such as emergency hospital admissions, are typically reviewed within 1-2 hours.
- Standard Requests: Standard requests, such as routine office visits, are typically reviewed within 2-5 business days.
- Complex Requests: Complex requests, such as surgeries or specialized treatments, may take longer to review, typically within 5-10 business days.
What to Expect After Submitting a Prior Auth Request
After submitting a prior auth request, providers can expect the following:
- Approval: If the request is approved, Arkansas BCBS will issue a prior auth approval letter, which includes the approved service or treatment and any conditions or limitations.
- Denial: If the request is denied, Arkansas BCBS will issue a denial letter, which includes the reason for denial and any appeal instructions.
- Request for Additional Information: If additional information is needed, Arkansas BCBS will contact the provider to request the necessary information.

Appealing a Prior Auth Denial
If a prior auth request is denied, providers can appeal the decision by following these steps:
- Review the Denial Letter: Review the denial letter to understand the reason for denial.
- Gather Additional Information: Gather any additional information or documentation that may support the appeal.
- Submit the Appeal: Submit the appeal to Arkansas BCBS, either online or by phone.
Arkansas Blue Cross Blue Shield Prior Auth Appeal Process
The prior auth appeal process typically involves the following steps:
- Initial Review: Arkansas BCBS will review the appeal and make a determination within 3-5 business days.
- Peer Review: If the appeal is denied, it will be reviewed by a peer reviewer, who will make a determination within 5-10 business days.
- Final Determination: The final determination will be communicated to the provider in writing.

We hope this article has provided a comprehensive guide to the Arkansas Blue Cross Blue Shield prior auth form and process. If you have any questions or need further assistance, please don't hesitate to comment below or share this article with others.
What is prior authorization (prior auth)?
+Prior authorization (prior auth) is a healthcare process where a patient's insurance provider reviews and approves a treatment or service before it is rendered.
Why is prior auth important?
+Prior auth is essential for patient safety, cost savings, and quality of care.
What services require prior auth with Arkansas BCBS?
+Services that may require prior auth with Arkansas BCBS include inpatient hospital services, outpatient services, pharmacy services, and durable medical equipment (DME).